COVID-19 Transmission within two Family Clusters by Presymptomatic Carriers in Uganda, May 2020
Daniel Eurien1,2, Bernadette Basuta Mirembe1,2, Godfrey Nsereko1,2, Denis Okethwangu1,2, Claire Biribawa1,2, Dativa Maria Alidekki1,2, Atek Atwine Kagirita1, Issa Makumbi1, Henry Kyobe3, Felix Ocom1, Alex Riolexus Ario1,2
1Ministry of Health, Kampala, Uganda, 2Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda, 3Uganda People´s Defence Forces, Kampala, Uganda, 4Uganda National Institute of Public Health, Kampala, Uganda
&Corresponding author
Danile Eurien, Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda, P.O. BOX 7072. euriend56@gmail.com
Introduction:
Coronavirus Disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It has spread globally, facilitated by travel. Family clusters have been identified as one of the facilitators of community spread. We investigated two family clusters in Eastern Uganda to identify the source of infection and recommend control measures.
Methods:
We investigated potential COVID-19 exposure events in two family clusters referred in this paper as family A and family B. We interviewed eight members of family A and two from family B at Soroti and Mbale Regional Referral Hospitals respectively between 23-30 May, 2020. Information on epidemiological, demographic and clinical data were collected using a structured questionnaire. Throat-swab specimens were obtained from all patients and closely monitored until patient discharge. Confirmation of SARS-CoV-2 was by RT-PCR test.
Results:
The two family clusters of COVID-19 infection resulted from the introduction of the virus from two respective heads of household who traded in livestock in South Sudan. The index case of family A (patient A1) generated seven secondary cases, all of whom shared an enclosed setting within one-meter distance with A1. The secondary cases of family A did not show any symptoms. Three household members who did not share an enclosed setting with A1 tested negative. The index case of family B (patient B1) generated four secondary cases. The four family members who tested positive were B2 (wife), B3 (daughter), B4 (son), and B5 (daughter). The only two household members (B6 and B7) who slept in a separate room did not test positive. All members of family B did not have symptoms at the time of testing.
Conclusion:
We found that two family clusters of COVID-19 infection were likely introduced by two heads of household who traded in livestock in South Sudan. Our findings show that close contact in enclosed settings within the family can amplify transmission of the COVID-19. We recommend testing and quarantine for cross-border traders before they return home, and limiting close contact within family settings to reduce spread. We recommend further investigation to better understand the source of infection for cross border traders.
Introduction

As of May 31, 2021, the World Health Organization (WHO) reported a total of 169,597,415 confirmed cases of coronavirus disease 2019 (COVID-19), including 3,530,582 deaths. COVID-19 is caused by a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; previously known as 2019-nCoV) [1, 2]. The number of cases of COVID-19 has grown significantly and has spread to all countries in the world [3]. The WHO characterized the COVID-19 epidemic as a pandemic on March 11, 2020 [4]. During the start of the COVID-19 pandemic, imported cases accounted for the highest proportion of total incidence in many countries around the world [3]. Uganda registered its first COVID-19 case on March 21, 2020, and by May 29, 2020, it had registered 329 COVID-19 cases, with the majority, 64% (210/329) among trans-border truck drivers. The Elegu border crossing during the week of 23-29 May 2020 accounted for 58% (90/156) of all the imported COVID-19 cases into Uganda [5].
The SARS-CoV-2 virus is highly infectious and has a strong ability to transmit from human to human. Evidence of human-to-human transmission was first reported in a family cluster of six members in China [
6,
7]. Person-to-person transmission in family clusters contributed to the exponential increase in the number of cases in China. In Beijing, family clusters were the main mode of person-to-person transmission accounting for 57.6% of the total confirmed cases [
8,
9]. These family clusters of COVID-19 infections reported in China were associated with recent travel of family members to areas with high transmission of COVID-19 [
6-9]. Therefore, early detection of family clusters of COVID-19 infection is important to prevent the further spread of the epidemic.
We report two family clusters of COVID-19 transmission and clinical features in two districts in Eastern Uganda, following the return of two family heads who plied their livestock trade in local markets in South Sudan.
Methods


Following the detection of the first COVID-19 case in Uganda on 22 Mar 2022, the government initiated steps to screen and test travellers arriving into the country from abroad. However, long-distance truck drivers were allowed passage to bring essential goods into the country or to transit to neighboring countries after taking a COVID-19 test at the border crossing point. On 14 May 2020, the National Rapid Response Team (NRRT) received information from a surveillance officer of Gulu District of two truck drivers whose results returned positive. The two truck drivers had been tested at the point of entry and allowed to proceed to their destinations before receiving results. The National COVID-19 Incident Management Team deployed a team of NRRT epidemiologists to support the district to investigate the suspected COVID-19 cluster. By the time the team started the investigation, other family members of the two truck drivers also showed symptoms of COVID-19.
We included two families in this study; with a total of sixteen family members; eleven from family A and five from family B. The index case in each family had a business trip to Juba, South Sudan. At the time of investigation, index case of family A was isolated at Mbale Regional Referral Hospital (RRH), and the one of family B was isolated at Gulu RRH.
Cluster investigation
We interviewed eight family members from family A and two family members from family B from 23-30 May, 2020 using a standard questionnaire at Soroti and Mbale Regional Referral Hospitals. We asked respondents about their potential exposure events 14 days before testing positive. The two hospitals were among the 14 hospitals designated by the Ministry of Health for the treatment of COVID-19. All patients were diagnosed as SARS-COV-2 positive by the Uganda Virus Research Institute (UVRI). Throat-swab specimens from the upper respiratory tract were obtained from all patients, maintained in viral transport medium, and shipped to UVRI. Confirmation of SARS-CoV-2 was by reverse transcriptase-polymerase chain reaction (RT-PCR) test.
Epidemiological and Clinical characteristics and laboratory testing
Additionally, epidemiological, demographic, and clinical data were collected through a review of medical records. Clinical data and laboratory testing results were closely monitored until 30 May, 2020. On day 10 of patient monitoring, laboratory confirmation of SARS-CoV-2 was carried out by UVRI as a precondition for patient discharge. Briefly, throat-swab specimens from the upper respiratory tract were obtained from all patients on day10 in admission and maintained in viral-transport medium to UVRI.
The index case of family A was isolated at Mbale Regional Referral Hospital (RRH), and the one of family B was isolated at Gulu RRH. All the eleven patients were diagnosed as SARS-CoV-2 positive using the Uganda Ministry of Health testing algorithm and were isolated and managed at Soroti RRH.
Ethical consideration
This was a public health emergency and the SARS-COV-2 Incident Management Team (IMT) of the Ministry of Health (MoH) gave the directive to conduct epidemiological investigations into clusters driving the spread of SARS-CoV-2 infection in the country. The investigation directive from MoH applied to all confirmed cases; however, we sought verbal consent from respondents in their local language during data collection. Participants were told that their participation was voluntary and that there would be no negative consequences if they refused to participate (none declined). During data collection, respondents were assigned unique identifiers instead of names to protect their confidentiality. Information was stored in password-protected computers and was not shared with anyone outside the investigation team. As this was a public health emergency, disclosure of patient information for the purposes of contact tracing was limited to the minimum needed to conduct contact tracing activities.
Results


Family A
On 13 May 2020, the index case (father) of family A (referred to here as patient A1) returned from South Sudan through Elegu point of entry where he had spent 5 days selling goats
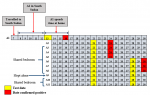
Table 1. Following government policy at the time of testing everyone entering the country, A1 was subjected to a throat swab for COVID-19 at Elegu border crossing that same day and the sample was shipped to Kampala (approx. 400km away). A1 reported no symptoms at the time of testing. He arrived at his home in Kumi District, about 350km away at 8:00pm on the same day. He shared a meal and later led a prayer with 10 family members including A2 (wife), A3, A4, A5, A6, A7, A8, A9 (daughters), A10 (son), and A11 (“turn man”-person who supports truck drivers during the journey). On 14 May 2020, A1 went to the neighbouring town (20km) to supervise the construction of his house, after which he returned home at 6:00 pm and participated in the same family ritual of praying together and having dinner with the 10 family members in the living room. A1 and A2 slept on one bed; A3, A4, A5, and A6 slept in one room, A10, and A11 shared another room; while A9 slept alone because she was asthmatic.
On 15 May, A1 traveled to Mbale (55km) to buy construction materials and returned home that evening and did the usual family ritual of eating together and leading a prayer before going to bed. On 16 May, he drove to his construction site along with his family including (A2, A3, A4, A5, A6, A8, A9, and A10) in a double cabin pick-up truck. A2 sat on the co-driver´s seat, A3, A4, A5, A6 sat in the middle cabin while, A8, A9, and A10 sat in the truck cargo bed. The Kumi District Rapid Response Team (DRRT) received positive results of A1 who was supervising his construction work at the time. He was informed by the DRRT about the positive results and immediately evacuated to the nearest isolation unit in Mbale RRH while members of his family were returned home by another driver who was subsequently home quarantined with the rest of the family
Figure 1.
On 21 May, the 10 members of A1´s family´s samples were taken and on 24 May 2020, results of A2, A3, A4, and A5 returned positive for COVID-19, while the rest tested negative. All the 10 family members were tested as high-risk contacts of A1 and non-reported any symptom at the time of testing. On 28 May, A10 exhibited flu-like symptoms, prompting the surveillance team to retest all family members who tested negative in the first test. On 30 May 2020, results of A6, A7, and A8 returned positive. The third tests of A9, A10, and A11 on 9th June 2020 were negative and subsequently discharged from quarantine
Figure 1.
Family B
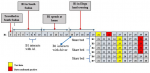
On 3 May 2020, the index case (father) of family B (referred to here as patient B1) travelled to South Sudan through Elegu land border crossing
Figure 2 where he spent 7 days selling his goats at a market in Juba, South Sudan. B1 interacted with A1 in the same market in South Sudan between 8th and 9th since they were business partners. He arrived home in Soroti on 10 May and spent five days with his family of six including B2 (wife), B3 (daughter), B4 (son), B5 (daughter), B6 (son), and B7 (daughter). B1´s driver returned to South Sudan on 11 May 2020 with new stock for sale. B1 returned to the Elegu border on 16 May 2020, where he interacted with his driver who had returned from South Sudan and tested on entry the same day. The driver´s results returned positive on 18 May 2020 prompting surveillance teams to trace B1 as one of the high-risk contacts. He was put in institutional quarantine and his sample was taken on 21 May 2020. His results returned positive on 23 May, 2020 and was evacuated to Gulu Regional Referral Hospital where he was managed together with his driver. Both B1 and his driver reported not having any symptoms at time of testing. The surveillance teams at the Elegu border crossing contacted the Soroti DRRT to quarantine and test B1´s family members
Figure 2. Four family members tested positive on 29 May 2020 including B2 (wife), B3 (daughter), B4 (son), and B5 (daughter). All family members reported no symptoms at the time of testing. During the time B1 was home, he shared a bed with B2 and B3 (9 months daughter); B4, B5, B6, and B7 shared one room. B4 and B5 shared one bed, while B6 and B7 also shared a bed
Figure 3.
Discussion


We investigated two family clusters of COVID-19 cases in two districts in Eastern Uganda along the Northern highway to South Sudan during 23-30 May, 2020. We found that COVID-19 was most likely introduced to the two families by the two heads of households who conducted livestock trade across the border in South Sudan. The Uganda-South Sudan border crossing (Elegu) was the highest source of imported cases of COVID-19 in Uganda with 51 cases reported between 4-10 May 2020, the week the two index cases made the crossing into Uganda [10,11]. The possible explanation for the high incidence of COVID-19 among cross-border traders is exposure to a more extensive social network, and likely crowded market places where the probability of contact with infected persons was high [12]. Additionally, market environments present a difficulty in enforcement of Standard Operating Procedures for the prevention of COVID-19 and have inadequate access to hand-washing facilities [13].
During the investigation period of May 2020, truck drivers from neighbouring countries were tested at the border and allowed to proceed to the country of destination if non-Ugandan, while Ugandan drivers were allowed to proceed to their homes. Those who turned positive were evacuated to the nearest isolation unit if Ugandan or handed over to their countries of origin if non-Ugandan. The two-family cluster index cases were Ugandan nationals who travelled to their families before getting results, therefore potentially exposed their family members to COVID-19.
These results on early transmission of COVID-19 facilitated by cross-border truck drivers were also observed in south African countries of South Africa, Botswana, and Zimbabwe [
14]. The free movement of the truck drivers therefore might have played a big role in the initial introduction of COVID-19 into households from where family clusters facilitated community-wide community transmission.
These two family clusters reinforced the importance of continuous testing of people entering the country at all points of entry regardless of whether they are symptomatic or not for COVID-19 since all the two index cases did not show any symptoms during screening at the border. The local truck drivers delivering cargo should therefore be quarantined awaiting their results before being allowed to see their families to avoid exposing their family members and other contacts.
Secondly, findings from our study are consistent with transmission dynamics shown in other similar studies that; close, prolonged contact between numerous people, in an enclosed space could facilitate the easy spread of the virus [
4-6]. This is well illustrated by family A in which despite the considerable interaction between family members in different outdoor activities, only three family members who did not become positive had the least close contact in enclosed spaces with the index cases. The spread of the virus was largely efficient among family members who spent more time in enclosed spaces with the index case including evening prayers in the living room, travelling together in an enclosed car, and secondary cases who slept in one room, “indicating that the duration of the interaction (or contact) in enclosed spaces was probably the main facilitator for extensive infection. Extensive transmission of COVID-19 through close contact with family members is documented in several countries including United States of America and China [
15-18]. Our study has some limitations. Because the index case patients could not disclose clear contact history, we could not establish the possible point of infection and therefore, epidemiologic links and clusters of cases might have been missed.
Our findings indicate that there is a need for continuous testing of everybody entering the country through every point of entry regardless of whether they are symptomatic or not. These findings also indicate that very close family interactions in closed settings are potential super spreading events that could drive the pandemic further. Therefore, active case finding and isolation in conjunction with comprehensive contact tracing and quarantine are useful for preventing imported cases from spreading the virus to their close family members. The provision of comfortable facilities for exposed contacts to quarantine or for mild cases to isolate away from their families could be a valuable strategy to limit onward transmission within households.
Conclusion


This family cluster investigation demonstrates how cross border traders introduced COVID-19 infections to their families. The results also show how close contact in enclosed settings within the family amplify transmission of COVID-19. Therefore, testing and quarantine is essential before letting cross border traders proceed to their families. Additionally, limiting of close contact within family setting is essential to reduce spread. Further investigation is needed to better understand the source of infection of cross border traders.
What is known about this topic
- Family clusters facilitated rapid spread of COVID-19 early on during the pandemic
- Adults introduced infections to younger persons within the household
- Increased interaction within closed setting in the household setting facilitate rapid spread of COVID-19
What this study adds
- Cross border traders contributed to early introduction of COVID-19 infection to their families in Uganda
- This study highlighted the need to revise the policy of testing and letting cross border traders proceed to their destinations
Competing interests


The authors declare no competing interests.
Authors' contributions


D.E, M.B.B, GN, DO, CB and DA collected the data, conceived the idea and drafted the manuscript, FO, AAR reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgments


We would like to thank the District Rapid Response Teams of Soroti, Kumi and Gulu, Soroti and Mbale Regional Referral Hospital teams for their roles in facilitating data collection and providing care to the cases. We also acknowledge the numerous personnel from the Central Public Health Laboratories and Uganda Virus Research Institute who helped with laboratory testing of cases.
Tables and figures


Table 1: Epidemiological and demographic characteristics of the two family clusters
Figure 1: Map showing trade route plied by A1 and B1
Figure 2: Detailed epidemiological timeline showing events during days of May 2020 of Family A. cluster. A1(Father); A2(Mother); A3(Daughter); A4(Daughter); 5(Daughter); A6(Daughter); A7(Daughter); A8(Daughter); A9(Daughter); A10(Son); A11(Turn boy)
Figure 3: Detailed epidemiological timeline showing events during days of May 2020 for Family B cluster B1 (Father); B2 (Mother,); B3 (Daughter); B4 (Son); B5 (Daughter); A6 (Son); A7 (Daughter)
References


- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet[Internet]. 2020 Mar[cited 2023 Feb 13]; 395(10229):1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3 . PubMed | Google Scholar
- World Health Organization (WHO). Weekly operational update on COVID-19 31 May 2021[Internet]. Geneva: WHO; 2021 May 31[cited 2023 Feb 13].
- Russell TW, Wu JT, Clifford S, Edmunds WJ, Kucharski AJ, Jit M. Effect of internationally imported cases on internal spread of COVID-19: a mathematical modelling study. The Lancet Public Health[Internet]. 2021 Jan[cited 2023 Feb 13]; 6(1): e12-20. https://doi.org/10.1016/s2468-2667(20)30263-2 . PubMed | Google Scholar
- Cucinotta D, Vanelli M. WHO declares COVID-19 a Pandemic. Acta Biomed[Internet]. 2020 Mar 19[cited 2023 Feb 13]; 91(1):157-60. https://doi.org/10.23750/abm.v91i1.9397. PubMed | Google Scholar
- Ministry of Health, Uganda. COVID-19 Resource Info Hub[Internet]. Uganda: Ministry of Health; 2020[cited 2023 Feb 13].
- Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR, Pacilli M, Fricchione MJ, Chugh RK, Walblay KA, Ahmed NS, Stoecker WC, Hasan NF, Burdsall DP, Reese HE, Wallace M, Wang C, Moeller D, Korpics J, Novosad SA, Benowitz I, Jacobs MW, Dasari VS, Patel MT, Kauerauf J, Charles EM, Ezike NO, Chu V, Midgley CM, Rolfes MA, Gerber SI, Lu X, Lindstrom S, Verani JR, Layden JE, Brister S, Goldesberry K, Hoferka S, Jovanov D, Nims D, Saathoff-Huber L, Hoskin Snelling C, Adil H, Ali R, Andreychak E, Bemis K, Frias M, Quartey-Kumapley P, Baskerville K, Murphy E, Murskyj E, Noffsinger Z, Vercillo J, Elliott A, Onwuta US, Burck D, Abedi G, Burke RM, Fagan R, Farrar J, Fry AM, Hall AJ, Haynes A, Hoff C, Kamili S, Killerby ME, Kim L, Kujawski SA, Kuhar DT, Lynch B, Malapati L, Marlow M, Murray JR, Rha B, Sakthivel SKK, Smith-Jeffcoat SE, Soda E, Wang L, Whitaker BL, Uyeki TM. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. The Lancet[Internet]. 2020 Apr[cited 2023 Feb 13]; 395(10230):1137-44. https://doi.org/10.1016/S0140-6736(20)30607-3 . PubMed | Google Scholar
- Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Xing F, Liu J, Yip CCY, Poon RWS, Tsoi HW, Lo SKF, Chan KH, Poon VKM, Chan WM, Ip JD, Cai JP, Cheng VCC, Chen H, Hui CKM, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet[Internet]. 2020 Feb[cited 2023 Feb 13]; 395(10223):514-23. https://doi.org/10.1016/S0140-6736(20)30154-9 . PubMed | Google Scholar
- Zhang H, Chen R, Chen J, Chen B. Covid-19 Transmission Within a Family Cluster in Yancheng, China. Front Med[Internet]. 2020 Jul 3[cited 2023 Feb 13]; 7:387. https://doi.org/10.3389/fmed.2020.00387. PubMed | Google Scholar
- Liu Z, Wu Q, Zou Z, Yao Y, Cai J, Liu T, Yang Z, Liu Q. Investigation of a family cluster outbreak of COVID-19 indicates the necessity of CT screening for asymptomatic family members in close contact with confirmed patients. J Thorac Dis[Internet]. 2020 Jul[cited 2023 Feb 13]; 12(7):3673-81. http://dx.doi.org/10.21037/jtd-20-955 . PubMed | Google Scholar
- Bajunirwe F, Izudi J, Asiimwe S. Long-distance truck drivers and the increasing risk of COVID-19 spread in Uganda. International Journal of Infectious Diseases[Internet]. 2020 Sep[cited 2023 Feb 13]; 98:191-3. https://doi.org/1016/j.ijid.2020.06.085 . PubMed | Google Scholar
- The Independent. South Sudan new hotspot, 21 truck drivers test COVID-19 positive[Internet]. Kampala (UG): The Independent; 2020 May 27[cited 2023 Feb 13].
- Usman IM, Ssempijja F, Ssebuufu R, Lemuel AM, Archibong VB, Ayikobua ET, Aruwa JO, Kembabazi S, Kegoye ES, Ayuba JT, Okeniran OS, Echoru I, Adeoye A, Mujinya R, Nankya V, Kasozi KI. Community Drivers Affecting Adherence to WHO Guidelines Against COVID-19 Amongst Rural Ugandan Market Vendors. Front Public Health[Internet]. 2020 Jul 3[cited 2023 Feb 13]; 8:340. https://doi.org/10.3389/fpubh.2020.00340. PubMed | Google Scholar
- Megersa K. The Informal Sector and COVID-19 in Sub-Saharan Africa[Internet]. Brighton, UK: Institute of Development Studies. 2020[cited 2023 Feb 13].
- Leslie J, Schmidt-Sane M. Key Considerations: COVID-19 RCCE Strategies for Cross border Movement In Eastern And Southern Africa[Internet]. UK: Institute of Development Studies; 2020[cited 2023 Feb 13].
- Diao K yue, Zhang X chun, Huang S, Wang H lun, Gang Y dong, Deng Y ping, Han P lun, Pang T, Yu J ling, Guo Y kun, Yang Z gang. Features of family clusters of COVID-19 patients: A retrospective study. Travel Medicine and Infectious Disease[Internet]. 2021 Jan[cited 2023 Feb 13]; 39:101950. https://doi.org/10.1016/j.tmaid.2020.101950 . PubMed | Google Scholar
- Edwards E. Family clusters: A common pattern for how the coronavirus spreads Close contacts - especially people living under the same roof - are at risk[Internet]. NBC News. NBC Universal; 2020 March[cited 2023 Feb 13].
- Lin G tian, Zhang Y hua, Xiao M fang, Wei Y, Chen J ni, Lin D jiong, Wang J chong, Lin Q yu, Lei Z xian, Zeng Z qiong, Li L, Li H ai, Zheng Y, Li Q qiong, Zhen H zhen, Jin Y ming, Wu Q xia, Zhang F, Xiang W. Epidemiological investigation of a COVID-19 family cluster outbreak transmitted by a 3-month-old infant. Health Inf Sci Syst[Internet]. 2021 Jan 18[cited 2023 Feb 13]; 9(1):6. https://doi.org/10.1007/s13755-020-00136-2. PubMed | Google Scholar
- Liu T, Gong D, Xiao J, Hu J, He G, Rong Z, Ma W. Cluster infections play important roles in the rapid evolution of COVID-19 transmission: A systematic review. International Journal of Infectious Diseases[Internet]. 2020 Oct[cited 2023 Feb 13]; 99:374-80. https://doi.org/10.1016/j.ijid.2020.07.073 . PubMed | Google Scholar