Analysis of Abortion Cases Data at the Referral Hospital of Haho Health District, Notsè - Togo, 2012 - 2017
Agballa Mébiny-Essoh Tchalla Abalo1,&, Essona Matatom Akara1,2, Hamadi Assane3, Degnanou Komi2, Edem Kpeglo2, Bernard Sawadogo4, Simon Antara4
1Direction Préfectorale de la Santé de Haho, Notsè, Togo, 2Centre Hospitalier Préfectoral de Notsè, Togo, 3Division de la Surveillance Intégrée des Urgences Sanitaires et de la Riposte, Lomé - Togo, 4African Field Epidemiology Network (AFENET)
&Corresponding author
Agballa Mébiny-Essoh Tchalla Abalo, Ministry of Health and Public Hygiene, Haho Health District Directorate, Referral Health District Hospital, N°1 National Street, Notsè, Togo. tchanaldinio@yahoo.fr, tchanaldinio1234@gmail.com
Introduction:
More than 95 percent of unsafe abortions occur in developing countries and contribute to 4.70 percent to 13.20 percent of maternal deaths. Abortions’ magnitude and characteristics are unknown at Notsè hospital yet these parameters are critical for effective planning of interventions and to mobilize resources for abortion management. We aimed to describe data quality, socio-demographic and clinical features of abortions cases.
Methods:
We conducted a descriptive study based on secondary data analysis of abortion cases admitted at Notsè hospital from January 2012 to December 2017. Data Completeness (DC) was used to classify data quality as Good: DC≥80%, Fair: 50%≤DC<80% or Poor: DC<50%. Medical files were reviewed to collect sociodemographic and clinical data. We performed descriptive analysis using Epi-info-7 software.
Results:
Over the study period, 760 abortions cases were admitted. Among the 34 study variables 26.47% (9/34) were of poor quality and 63.16% (12/19) of required data were of good quality. Overall women mean age ranged from 23.97 ±6 years in 2012 to 26.8 ±7.60 years in 2017 (p=0.026) and those aged from 18 to 30 represented 69.8% (505/724). Seventy percent of women were from rural area. Housewives represented 53.8% (388/721) and 10.5% (76/721) were pupils. Per 1,000 women aged 15-49, abortion ratio varied from 23 in 2012 to 45 in 2017. In medical history 94.56% (644/681) of cases had experienced at least one abortion in the past and 70.53% (474/672) of abortions occurred before 17 weeks of gestation. Among women admitted with metrorrhagia, 9.59% (52/542) had received blood transfusion. Malaria was diagnosed and treated in 30.93% of the 333 tested women. No death was recorded.
Conclusion:
Abortions are frequent, mainly in women with malaria and hemorrhagic complications. The quality of some required data was poor. Caregivers’ training and strategies to improve access to malaria care for pregnant women and increase access to contraceptive methods should be strengthened.
Introduction

Abortions still remain one of the main causes of high maternal mortality in many healthcare systems around the world [1-5]. The real incidence of the phenomenon across world regions is disparate and has varied between 27 abortions per 1,000 women aged 15-44 in developed regions, and 35 abortions per 1,000 women aged 15-44 in developing regions in 2017 [1,6]. These variations in the incidence of the phenomenon of abortions from one region of the world to another is partly related to the legal context regarding abortions and to socio-cultural considerations in these regions [6,7-9]. While in developed countries, abortions are a little more controlled, in low and middle-income countries, particularly in Africa, abortions are carried out under unsafe conditions [10-12]. Every year, about 56 million abortions occur in women of childbearing age, and nearly half of them happen to be unsafe [13]. In Africa, 35% of pregnancies are unwanted, often leading to abortions, and 3 out of 4 abortions are at risk of any complication [14]. The cost of abortions phenomenon for healthcare systems in Africa is huge and is estimated to be about 171 million US $ annually [14]. In the current context of promoting contraceptive measures as an approach to reduce the incidence of abortions in general and unsafe abortions in particular, statistics are different.
In Togo, the real incidence of the phenomenon is underestimated [
6] and the available data on abortions are from hospitals and health facilities registers. According to the non-published annual reports, the total number of abortion cases recorded in Togo was 7,032 in 2013 and 7,695 in 2016 with respective proportions of induced abortions of about 9% and 21%. Over the two periods, in the Plateaux region where the Haho district is located, respectively 1,966 and 1,878 cases of abortions were reported of which 30% and 25% were induced.
The knowledge of the epidemiological profile of any disease or health condition including abortion is crucial for planning of control strategies and mobilizing resources. Abortion cases have been managed at the hospital of Notsè for several decades, but there is an insufficiency of the magnitude and the profile of women affected. This study aims to describe the data quality, the socio-demographic and clinical profile of abortions at the referral hospital of Haho district (Notsè hospital) in Togo from 2012 to 2017.
Methods


Study settings
This study was conducted in the department of Gynecology and obstetrics of Haho health district referral hospital, the only one in the district where abortion can be managed in safe conditions. Haho health district is located in Plateaux health region, between N06 ° 26 '47, 0´ and E001 12' 32, 0´ with 288,832 inhabitants in 2017 including 72,208 women of childbearing age. Less than 50% of childbearing age women live within an hour drive of the district referral hospital (Notsè Hospital). Until December 2017, the medical staff of the department of Gynecology and obstetrics was constantly composed of at least one (01) surgeon who can take care of severe complications of abortions, at least two (02) nurses in anesthesiology, and at least 13 midwives. This staff was trained, qualified and had the least of the technical facilities required to take care of abortions and their complications.
Data on abortion cases admitted to Notsè Hospital are recorded in medical records on hard-copies that the staff use to prepare monthly reports.
Study design and period
This was a descriptive study carried out from January to April 2018 and covered cases of abortion admitted in Haho health district referral hospital from January 2012 to December 2017.
Study population
The study included all cases of abortions admitted and managed in Haho health district referral hospital. Was considered as a case of abortion, any expulsion of all or part of the products of conception prior to the 20th week of gestation in a woman of childbearing age who was admitted in Haho health district referral hospital from January 2012 to December 2017.
Study variables and definitions
The following variables have been described:
- Completeness and inconsistency of data and required variables. Given that the study focused on secondary data, data quality was assessed by considering the components of data completeness and inconsistency. Completeness was defined as the percentage of data available for each variable, and inconsistency as the existence of a non-logical relationship between the data for two or more variables for an abortion case. Required data were defined as data that could be used to describe women´s social characteristics, their medical history, the age of the pregnancy, the clinical features that may constitute an emergency. Completeness was classified as “Good” when the proportion of available data of a variable was equal or more than 80% (≥ 80%), as “Fair” when it was equal or more than 50% and less than 80% (50% ≤ Value < 80%) and as “Poor” when it was less than 50% (< 50%).
- Sociodemographic characteristics: age, sex, marital status, occupational category, living area (rural or urban), the type of sexual partner,
- Clinical characteristics: history of abortion, parity and history of pregnancy, anatomoclinical type of abortion, clinical presentation at entrance, therapeutic means used in management of the cases, the blood Rhesus type, the abortion product nature (complete or incomplete) and the presence of malaria.
Malaria diagnosis and blood rhesus grouping
In order to determine whether or not the women admitted were affected by malaria and to treat them, they underwent a biological malaria diagnosis. Malaria was diagnosed using “One step Malaria Antigen P.f (HRP-II) Rapid Test®” of SD BIOLINE. Microscopic examination of the thick blood drop was also used. A woman was considered to have malaria if one of these tests was positive.
For blood rhesus group identification, the Beth Vincent agglutination test was used.
Data collection
A data abstraction tool was designed for this study. Through a systematic review of both admission and hospitalization registers, patients´ clinical records, the available data were extracted and reported on the designed tool.
Data processing and analysis
The data collected were processed in Microsoft Excel 2013 using a predesigned spreadsheet. The database was then cleaned by removing outliers that could not be corrected, and was imported into Epi Info version 7.2.1.0 for statistical analysis. Age variable was encoded as age groups; the history of pregnancy and delivery in gravidity and parity respectively. In univariate analysis, frequencies, proportions, mean, Standard Deviation and ratios were calculated for the different variables and then presented in tables or graphs. To explore the similarity or the difference between the values of the study variables, Student's t-test was used to compare the mean age of abortion cases between two years and Pearson's Chi2 test to compare proportions. For a p-value of less than 0.05, the difference between the values of the measured variables was considered significant.
Ethical consideration
The study was approved by the Togo National Department of Disease control and Prevention. Data were processed in anonymous and in strict confidentiality.
Results


Medical records data quality
There were 34 variables for this study, of which 26.47% (9/34) were of poor completeness. Among the 19 variables identified as required for this analysis, data completeness varied from 0,00% for prophylaxis of Anti-D immunoglobulin to 100% for cervical injuries, intravaginal foreign bodies, therapeutic means used and abortion outcomes. Completeness of required data
Table 1 were good in 63.16% (12/19) and poor in 36.84% (7/19). No inconsistent data or information was found during the medical files reviewing.
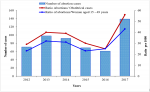
Abortion magnitude at the department of Gynecology and obstetrics
Over the six years of study period, 760 abortions were recorded with an overall ratio of 30 abortions per 1000 women of childbearing age ranging from 23 in 2012 to 45 in 2017. The overall ratio of abortion cases reported to all obstetrics admissions was 37 abortions per 1,000 obstetric admissions and was ranged between 29 in 2013 and 56 in 2017
Figure 1.
Socio-demographic characteristics
The overall mean age of women admitted for abortion was 26 years ± 7 years. The mean ranged from 23.97 ± 6 years in 2012 to 26.8 ± 7.60 years in 2017 (p = 0.026). Women aged less than 18 accounted for 7.73% (56/724) followed by women aged above 30 for 22.50% (163/724) and women aged from 18 to 30 represented 69.80% (505/724). Seventy percent of women were living in rural areas. According to their occupational characteristics, housewives, workers of informal sector and students represented respectively 53.8% (388/721), 33.8% (244/721) and 10.5% (76/721)
Table 2. Among the 185 cases that had their marital status available, 42 (22.70%) were single, 142 (76.76%) were married and one (0.54%) was a widow. About 81.62% of them (151/185) had a regular sexual partner and 18.40% (34/185) had a casual sexual partner. Among women who had a casual sexual partner, 88.24% (30/34) were single, 8.82% (3/34) married and 3% (1/34) widow. According to quarters of the year, 23.51% (158/672) of abortion occurred in the first quarter, 23.81% (160/672) in the second, 30.95% (208/672) in the third and 21.73% (146/672) in the fourth.
Clinical characteristics
In their medical history, 94.56% (644/681) of women, already had at least one abortion in the past, with a minimum of one abortion in the past found in 568 cases of whom 56 (9.86%) were students and a maximum of 6 abortions in the past were found in two (02) women
Table 2. Of the 681 women for whom pregnancy history data were available, 28.05% (191/681) were primigravida, 34.06% (232/681) were paucigravida and 37.88% (258/681) were multigravida. According to their parity, 32.45% (221/681) were nulliparous, 17.18% (117/681) were primiparous, 25.84% (176/681) were pauciparous and 24.52% (167/681) were multiparous. From 2012 to 2017, according to the history of pregnancy, the proportion of multigravida cases who had experienced abortions increased from 29.87% (23/77) to 36.96% (68/184) with p = 0.27 while the proportion of primigravida cases decreased from 25.97% (20/77) to 25.00% (46/184) with p = 0.86. Considering the parity, from 2012 to 2017, the proportion of pauciparous and multiparous cases who had experienced abortions increased respectively from 24.68% (19/77) to 28.26% (52/184) with p = 0.55 and 18.18% (14/77) to 23.37% (43/184) with p = 0.35 while that of nulliparous and primiparous women decreased from 33.77% (26/77) to 27.72 % (51/184) with p = 0.32 and from 23.38% (18/77) to 20.65% (38/184) with p = 0.62 respectively
Figure 2.
According to the anatomoclinical presentation of the abortion product, 0.15% (1/672) were subclinical, 32.89% (221/672) were ovular, 47.47% (319/672) were embryonic and 19.49% (131/672) were fetal. Of the cases of embryonic abortion, 70% occurred in women between 18 and 30 years old while among ovular´s, 68.1% occurred in women of the same age group. The three first clinical manifestations recorded at admission were metrorrhagia, pelvic pain and fever in respectively 71.32% (542/760), 23.72% (180/759), and 9.63% (73/758) of the cases. Among women admitted for metrorrhagia 9.59% (52/542) presented complication of decompensated anemia. Intravaginal foreign bodies were found in 0.79% (6/760) of the cases and 0.66% (5/760) of the cases had cervix injuries. Among 333 women tested for malaria, 30,93% were positive. The therapeutic management of the cases consisted in misoprostol administration in 5.67% (43/759), oxytocin in 49.61% (377/760), blood transfusion in 7.50 % (57/760), Manual Vacuum Aspiration (MVA) in 8.84% (67/758), anti-tetanus serum in 2.25% (17/758), anti-malaria drugs in 16.05% (122/760), antibiotics in 47.37% (360/760), analgesics in 43.95% (334/760). For the 7.67% (37/482) of women who had a rhesus negative blood no data concerning anti-D immunoglobulin prophylaxis were available. There was no maternal death related to abortion during the study period.
Discussion


Over the six year of study period, the ratio of abortion remained high indicating that abortion is common at the Notsè hospital. The analysis findings showed an increase in the ratio of abortion cases by almost 50% from 2012 to 2017.
This high ratio is similar to that in West African countries, which is 31 per 1000 women of childbearing age, but lower than the ratio of the Northern and Southern African countries which is respectively 38 and 34 per 1000 women [
6]. This difference can be explained by the methods of estimation of abortion cases, the legal and socio-cultural specificities surrounding abortion phenomenon in each of these parts of Africa, inequalities in accessing family planning methods by women of childbearing age from region to another [
12,
15-20]. In Togo, the law No 2007 - 005 of 10th January 2007 on reproductive health restricted the practice of intended abortions to the circumstances of rape, incest, fetal malformation and serious consequences on the life of the pregnant woman. Abortion is not well perceived and accepted by the community in Togo and is considered as a shameful act, especially when it concerns women living in couple as in this study. Women who have abortion are considered to be those who cheat on their spouses, or who are unable to carry a pregnancy to term.
Slightly more than two-thirds of the cases were from rural areas. The mean age of the cases over the six years was 26 years and most of them were aged 18-30 years. According to the pregnancy history, paucigravida and multigravida women were the most represented and at least 80% had already experienced an abortion at least once in the past. These data show that in Haho district, abortions occur mostly among women who do not have easy access to health care and health education information about abortion and who have knowledge of pregnancy. This observation corroborates the fact that the population of Haho is mainly composed by young people and living in rural areas. Some studies have, contrary to the current findings, shown that abortions most occur in urban areas [
21,
22]. Other studies have respectively found 26.7 years, 24.7 years and 22.4 years as mean age for their cases [
22-24].
The majority of abortions cases occurred among married women in 76.8% of the cases. According to Demographic and Health Survey (EDST III) conducted in Togo in 2013, 66% of childbearing women were married [
25]. Although the proportion of married women is considerable, the high proportion of abortion among married women, could be explained by the probable low recourse of single women to Notsè hospital for abortion. This trend is the same found in many other studies that were conducted in low- and middle-income countries that have similar demographic profiles as Togo [
26,
27]. In other studies, married women were less represented with respectively 44%, 13% and 44.8% [
23,
28,
29]. This difference could be related to studies designs, especially sites where data were collected and also the laws on abortion in these countries. Indeed, the nature of the abortion law influences abortion care services use particularly by the single women.
Most of abortions product were ovular or embryonic. The high frequency of abortions during these periods is thought to be due to elective termination of an unintended pregnancy [
6]. In this case, abortion happens as soon as possible before the pregnant woman's abdomen is visible. When it´s an intended pregnancy, this could be the result of morphological abnormalities of the uterus, cervix or hormonal abnormalities in the pregnant woman. In both cases, an infection, a trauma or other disease could contribute or be the cause of the expulsion of the product of conception. In our study more than one third of tested women were positive for malaria and this could be an infectious cause of the abortions.
Metrorrhagia was the main clinical manifestation at admission; this is because metrorrhagia is the most clinical manifestation encountered at Gynaeco-Obstetrics admission especially in abortion cases. The current findings have been observed in similar proportions in other studies [
30,
31]. The evacuation of the abortion product or its remains was most performed by using uterotonic drugs in this study compared to the use of other means of uterine evacuation [
28]. This high use of uterotonic drugs as uterine evacuation mean is in connection with the therapeutic algorithm in force during the study period for uncomplicated cases of abortion and the cases in this study happen to have been most of the time uncomplicated.
Over third quarter of study variables had good and fair completeness. Despite this acceptable level of completeness of most of the variables, some variables that could have helped describe more the phenomenon of abortion had no data; this concerned data related to the characteristics of spontaneous or induced, clandestine, safe or unsafe of the abortion. The absence of this data on medical records could be explained by the caregivers´ negligence of the importance to fill in these informations on medical records. The poor information on the unintended and intended nature of the abortion could also be explained by the fear of the patient to be misjudged or to be declared to her husband if she declares that it is an intended abortion. The restrictions on the conditions of intentional interruption of pregnancy by law No 2007 - 005 of 10th January 2007 may also explain this situation.
This study was based on a secondary data analysis over a retrospective period of six years. Actually, in such retrospective studies, limitations are related to data incompleteness and the inability to correct some outliers. Indeed, data related to intended or unintended pregnancies, spontaneous or induced abortion, the fact that the abortion process was carried out under safe or unsafe conditions, the use of contraceptive methods in women medical history were not available. To optimize data quality, outliers that could not be verified were removed from the final database.
Conclusion


Data completeness related to this study was acceptable in general, but some relevant data were not available due, partly, to the retrospective type of the study. Over the study period, abortions magnitude was high. Most of the women that experienced abortion was young, married, coming from rural areas and were admitted with metrorrhagia and pelvic pain. More than three quarter of abortion occurred at the first quarter of the pregnancy and the expulsion of the conception product was incomplete at admission. All women survived but Anti-D immunoglobulins was not administered in Rhesus-negative women to preserve their lives and their future pregnancies.
There is need to establish and adopt strategies to improve the filling of medical records especially for all relevant data as well as their archiving. The actions to improve data completeness could be to set up a specific record for abortion cases as well as the monitoring of the completeness of data on abortion case records. It´s also important to conduct a study on why abortions most occurred in married women. Midwives and others reproductive health caregivers should be trained on abortion cases management. The health district directorate should intensify communication across all peripheral health facilities within the catchment area of the Notsè referral district hospital on promoting family planning, contraceptives methods use and establish advocacy to implement mechanisms that could help increase geographical and financial accessibility of contraceptives methods. Strengthening communication and resource mobilization for malaria control and prevention in pregnant women could also contribute to reduce abortions magnitude and improve their management.
What is known about this topic
- Abortion magnitude is higher in low- and middle-income countries than developed countries
- Most cases of abortion occurred in unsafe conditions especially in Africa, Asia and Latin America
What this study adds
- This study provides the epidemiological profile of abortion cases admitted at Notsè hospital
- Findings are focused especially on Notsè hospital and could be used to plan, to reprioritize actions or enhanced abortion cases management and strategies to reduce abortion incidence in Haho health district
Competing interests


The authors declare no competing interests.
Authors' contributions


Tchalla Abalo Agballa Mébiny – Essoh: development of the protocol of the study, data collection, data processing and analysis, manuscript development and its reviewing. Akara Essona Matatom: data collection, data processing and analysis, manuscript development and it reviewing. Kpeglo Edem, Degnanou Komi, Hamadi Assane: data collection and manuscript reviewing. Sawadogo Bernard, Simon Antara: development of the protocol of the study and manuscript reviewing. All authors reviewed and approved the final manuscript version.
Acknowledgements


The authors thank the Disease Control and Prevention Directorate of Togo’s Ministry of Health, the Plateaux Health region directorate and the Department of Gynecology and Obstetrics of the Haho District Reference Hospital.
Tables and figures


Table 1: completeness of data essential to the analysis of abortion cases, Notsè referral hospital, 2012 - 2017
Table 2: sociodemographic and clinical characteristics of patients admitted for abortion, Haho referral district hospital, Notsè - Togo, 2012 - 2017
Figure 1: evolution of abortion number cases, abortion/obstetrical cases ratio and abortion/women aged 15 - 45 ratio, Haho district referral hospital, 2012 - 2017
Figure 2: evolution of abortion number cases and proportions among nulliparous, primiparous, pauciparous and multiparous, Haho district referral hospital, 2012 - 2017
References


- Ganatra B, Gerdts C, Rossier C, Johnson JrBR, Tuncalp Ö, Assifi A. Global, regional, and subregional classification of abortions by safety, 2010 - 2014: estimates from a Bayesian hierarchical model. Lancet 2017; (390):2372-8.https://doi.org/10.1016/S0140-6736(17)31794-4 . Google Scholar
- Marlow HM, Wamugi S, Yegon E, Fetters T, Wanaswa L, Msipa-Ndebele S. Women´s perceptions about abortion in their communities: perspectives from western Kenya. Reproductive Health Matters. 2014; 22(43):149-158.https://doi.org/10.1016/S0968-8080(14)43758-3 . Google Scholar
- Lema V, Rogo K, Kamau R. Induced abortion in Kenya: Its determinants and associated factors. East African Medical Journal. 1996; 73(3):164-68. Google Scholar
- Osiemo R. Unsafe abortion in Kenya. Tropical Doctor. 2005; 35(3):159-60. Google Scholar
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, Gülmezoglu AM, Temmerman M, Alkema L. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health. 2014; 2(6):e323-e333.https://doi.org/10.1016/S2214-109X(14)70227-X . Google Scholar
- Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion Worldwide 2017: Uneven Progress and Unequal Access. New York: Guttmacher Institute. 2018. Accessed March 2019. Google Scholar
- Boland R, Katzive L. Developments in Laws on Induced Abortion: 1998-2007, International Family Planning Perspectives. 2008; 34(3): 110-120. Google Scholar
- Izugbara C, Otsola K, Ezeh A. Men, women, and abortion in central Kenya: a study of lay narratives. Medical Anthropology. 2009; 28(4):397-425.https://doi.org/10.1080/01459740903304009 . Google Scholar
- Ndunyu L. Induced abortion amongst women in Kenya. Loyola Journal of Social Science. 2007; 21(1):9-27.
- Shah I, Ahman E. Unsafe abortion in 2008: global and regional levels and trends. Reproductive Health Matters. 2010; 18(36):90-101. https://doi.org/1016/S0968-8080(10)36537-2. Google Scholar
- Shah I, Ahman E. Unsafe abortion differentials in 2008 by age and developing country region: high burden among young women. Reproductive Health Matters. 2012; 20(39):169-73. https://doi.org/10.1016/S0968-8080(12)39598-0. Google Scholar
- N´Bouke A, Calvès A, Lardoux S. Facteurs associés au recours à l´avortement à Lomé (Togo) : analyse d´une séquence d´étapes menant à l´avortement. Cahiers québécois de démographie. 2016; 45(2):217-246.https://doi.org/10.7202/1040396ar . Google Scholar
- Parmar D, Leone T, Coast E, Murray S, Hukin E, Vwalika B. Cost of abortions in Zambia: a comparison of safe abortion and post abortion care. Global Public Health. 2017; 12(2):236-249.https://doi.org/10.1080/17441692.2015.1123747 . Google Scholar
- Vlassoff M, Walker D, Shearer J, Newlands D, Singh S. Estimates of health care system costs of unsafe abortion in Africa and Latin America. International perspectives on sexual and reproductive health. 2009; 35(3):114-121. Google Scholar
- Ahiadeke C. Incidence of induced abortion in southern Ghana. International Family Planning Perspectives, 2001 ; 27(2) :96-01. https://doi.org/10.2307/2673822. Google Scholar
- Pallikadavath S, Stones RW. Maternal and social factors associated with abortion in India: a population-based study. Int Fam Plan Perspect. 2006; 32(3):120-5. Google Scholar
- Cresswell JA, Schroeder R, Dennis M, Owolabi O, Vwalika B, Musheke M, Campbell O, Filippi V. Women's knowledge and attitudes surrounding abortion in Zambia: a cross-sectional survey across three provinces. BMJ Open; Mar 2016, 6(3): e010076.https://doi.org/10.1136/bmjopen-2015-010076 PubMed | Google Scholar
- Johnson-Hanks J. The lesser shame: abortion among educated women in southern Cameroon. Soc Sci Med. 2002; 55:1337-49. https://doi.org/10.1016/S0277-9536(01)00276-3. Google Scholar
- Webb D. Attitudes to “Kaponya Mafumo”: the terminators of pregnancy in urban Zambia. Health Policy Plan. 2000; 15:186-93.https://doi.org/10.1093/heapol/15.2.186 . Google Scholar
- Henshaw SK.Unintended pregnancy and abortion in the USA: Epidemiology and public health impact . Family Planning Perspectives, 1998, 30(1):24-29 & 46. Google Scholar
- Amiar L, Boukhorb S, Hmimou S, Soulaymani A, Mokhtari A, Soulaymani-Bencheikh R. Profil épidémiologique des avortements provoqués au Maroc, 1992 - 2014. European Scientific Journal. May 2018, 14(15): 1857 - 7881.
- Owolabi OO, Cresswell JA, Vwalika B, Osrin D, Filippi V. Incidence of abortion-related near-miss complications in Zambia: cross-sectional study in Central, Copperbelt and Lusaka Provinces. Contraception 2017; 95: 167-174.https://doi.org/10.1016/j.contraception.2016.08.014 . Google Scholar
- Prata N, Bell S, Holston M, Gerdts C, Melkamu Y. Factors associated with choice of post-abortion contraception in Addis-Abeba, Ethiopia. African Journal of Reproduction Health. 2011; 15(3):51-7. Google Scholar
- Mayi-Tsonga S, Diallo T, Litochenko O, Methogo M, Ndombi I. Prévalence des avortements clandestins au centre hospitalier de Libreville, Gabon. Bull Soc Pathol Exot. 2009; 102(4):230-232. Google Scholar
- Ministère de la Planification, du Développement et de l´Aménagement du Territoire, Direction Générale de la Statistique et de la Comptabilité Nationale, Ministère de la Santé, Togo. Troisième Enquête Démographique et de Santé (EDSR-III 2013 - 2014). WHO Afro. Accessed March 2020.
- Haddad LB, Nour NM. Unsafe abortion: Unnecessary Maternal Mortality. Rev Obstet Gynecol. 2009; 2(2):122-1. PubMed | Google Scholar
-
Yokoe R, Rowe R, Choudhury SS, Rani A, Zahir F, Nair M. Unsafe abortion and abortion-related death among 1.8 million women in India. BMJ Glob Health 2019; 4(3):e001491. https://doi.org/10.1136/bmjgh-2019-001491 . PubMed | Google Scholar
- Biney AAE. Exploring Contraceptive Knowledge and Use among Women experiencing Induced Abortion in the Greater Accra Region, Ghana. Bioline International 2011; 15:39. Google Scholar
- Moreau C, Trussell J, Desfreres J, Bajos N. Patterns of contraceptive use before and after an abortion: results from a nationally representative survey of women undergoing an abortion in France. Contraception. 2010; 82(4):337-44.https://doi.org/10.1016/j.contraception.2010.03.011 . PubMed | Google Scholar
- Laghzaoui O. Avortements non médicalisés: état des lieux à travers une étude rétrospective de 451 cas traités à l'hôpital militaire d'instruction Moulay Ismail Meknès, Maroc [Inventory of unsafe abortions: retrospective study of 451 cases treated in Moulay Ismail Military Hospital of instruction, Meknes, Morocco]. Pan Afr Med J. 2016 May 25; 24:83. French.https://doi.org/10.11604/pamj.2016.24.83.8624 PubMed | Google Scholar
- Mwetaminwa SG, Kyembwa MM, Taji LS, Asimwe A, Okenge P, Katenga BG. Prévalence, complications et issue des avortements clandestins dans la ville de Kisangani en République Démocratique du Congo. International Journal of Innovation and Applied Studies. 2018; 25(1):403-409. Google Scholar