Environmental and psychosocial predictors of breast cancer screening among women in Gwagwalada Area Council, Abuja, North Central, Nigeria
Abah Ukpojo Angela1,&, Adefisoye Adewole2, Olugbenga-Bello Adenike Iyanuoluwa1
1Department of Community Medicine, Ladoke Akintola University of Technology (LAUTECH), Ogbomoso, Nigeria, 2National Stop Transmission of Polio Program (NSTOP), African Field Epidemiology Network (AFENET), Nigeria Country Office, Abuja, Nigeria
&Corresponding author
Abah Ukpojo Angela, Department of Community Medicine, Ladoke Akintola University of Technology (LAUTECH), Ogbomoso, Nigeria. abahangela@gmail.com
Introduction:
Breast cancer (BC) is the leading cause of morbidity and mortality among women. Although screening is a known cost-effective strategy for reducing its burden, uptake remains sub-optimal. This study was designed to determine environmental and psychosocial predictors to uptake of screening services among women in Gwagwalada area council, Federal Capital Territory (FCT).
Methods:
A descriptive cross-sectional study was conducted, and 514 women aged ≥25 years were interviewed using a semi-structured interviewer administered questionnaire. Data on socio-demography, knowledge, practice, and environmental/psychosocial barriers to screening was collected. Data analysis was done using IBM Statistical Packages for Social Sciences version 23.
Results:
The mean age of respondents was 38.36±11.6years. 275(53.5%) had good knowledge while 239(46.5%) had poor knowledge about BC. Assessment of utilization of screening method showed that 115(22%) of respondents had ever conducted a Breast Self-Examination while 1(0.2%) had conducted a mammography. Poor access routes (aOR:0.29 (95% CI: 0.118-0.701)), high cost of screening (aOR:0.29 (95% CI: 0.133-0.620)) and long waiting hours (aOR:0.25 (95% CI: 0.107-0.567)) were identified environmental predictors. Fear of positive diagnosis (aOR:11.41 (95% CI: 3.157-41.270)), fear of being tagged promiscuous (aOR:0.07 (95% CI: 0.007-0.810)), deficiency in awareness programs (aOR:0.39 (95% CI: 0.160-0.960)) and not aware of screening age (aOR:0.29 (95% CI: 0.102 – 0.809)), were found to be psychosocial predictors of screening.
Conclusion:
Screening for breast cancer among women in Gwagwalada area council was influenced by environmental and psychosocial factors. Findings from this study points to a great need in increasing sensitization programs, screening sites and subsidizing cost of screening services.
Introduction

Breast cancer is the most frequently diagnosed and the leading cause of cancer death among females worldwide, with an estimated 1.7 million cases and 521,900 deaths in 2012. Breast cancer alone accounts for 25% of all cancer cases and 15% of all cancer deaths among females according to the Global Cancer Observatory report [1]. Although screening is a known cost effective strategy used in reducing the burden of breast and cervical cancer worldwide, its uptake particularly in developing countries is still abysmal [2]. Screening for early detection of the disease among Nigerian women is not a common practice in the country. Attitudes towards seeking health is poor leading to untimely or preventable death among women. It has been observed that socio cultural, religious, genetic and economic factors are responsible for this poor attitude [3-4]. Even though reasons for poor utilization have been explored in other parts of Nigeria, not much has been done in the Federal Capital Territory and little has been done in relation to environmental and psychosocial barriers to screening. Most studies also utilized qualitative approach in documenting perceived barriers to uptake of services, thereby getting group perception about the subject and not individual perceived barriers.
This study was therefore conducted among women in Gwagwalada area council of the Federal Capital Territory (FCT). It attempts to examine the level of knowledge on breast cancer; practice of screening and to identify environmental and psychosocial factors associated with poor screening uptake, thereby suggesting probable solutions/recommendations for policy decisions, assist in planning and implementation of effective breast cancer screening programs to reduce the mortality and morbidity resulting from the disease.
Methods


Study setting
This study was conducted in two wards (Kutunku and Gwagwalada central wards) of Gwagwalada area council. Gwagwalada Area Council of the Federal Capital Territory (FCT) is a rapidly growing satellite town with an area of 1069.589 km2 and a population figure of 158,618 people at the 2006 census. With a national population growth rate of 3.2% [
5], the total population of people in the area council is 238,885 as at 2019. According to Anne et. al [
6], women of child bearing age represent 24% of the total population, therefore a total of 52, 555 women of child bearing age are present in the study area. The inhabitants of the area council have different religious affiliations such as Islam, Christianity, and Traditional religions. The predominant occupations of the inhabitants of the town include farming and trading but a good proportion of the people are civil servants. The area council has forty-one health facilities (28 public and 13 private). Breast cancer screening services is provided by the University of Abuja Teaching hospital and six private health facilities.
Study Design
A cross sectional analytical survey research design was adopted to determine the environmental and psychosocial barriers to breast cancer screening among women aged 25 years and above in Gwagwalada Area Council, FCT, Abuja.
Eligibility criteria
Inclusion criteria for participants
Women aged 25 years and above residing in Gwagwalada Area Council, FCT for at least 6 months.
Exclusion criteria for participants
Women who have been diagnosed of breast cancer and women who met the inclusion criteria but were unavailable during the conduct of the study.
Sample size
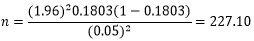
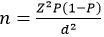
The sample size was determined using Fisher´s formula for estimating single proportions and the formula for estimating the minimum sample size. The standard normal deviation was set at a 95% confidence level, with the allowable margin of error of 5%. The equation for the Fisher´s formula:
Where:
n = minimum required sample size in population greater than 10,000, (n=52,555; Women of childbearing age in Gwagwalada Area Council)
Z = Standard normal variate for 95% confidence level, (Z = 1.96)
d = acceptable difference; using 5% (d = 0.05)
q = 1 - p
Based on documentation of previous study conducted in Nigeria by Okunowo et.al [
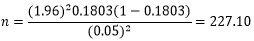
7], a proportion of 18.03% will be adopted in this study as the percentage of breast cancer screening uptake by women in Nigeria.
DEFF= Multiplying the sample size by 2 (Cluster design effect in conformity with WHO standard)
Minimum sample size (n) = 227.10 x 2 = 454.2
A 10% non-response rate was anticipated.
454.2+ 45.42= 499.62
A total of 517 questionnaires were administered for this study.
Sampling technique
A multistage sampling technique was employed in the selection of respondents.
Stage 1: A sampling frame of all the wards in Gwagwalada Area Council was documented. Using simple random technique by balloting, two of the total ten wards in Gwagwalada Area Council were selected. Kutunku and Gwagwalada central wards were selected for the study.
Stage 2: In the selected wards, two rural communities and two urban communities were also selected using simple random technique by balloting, from each of the wards. A total of 8 communities was used for the study. From Kutunku ward, New kuntuku and compensation layout were selected as urban communities and Old kuntuku as well as old Kaida were selected as rural communities. For Gwagwalada central ward, Angwan Tiv and Passo were selected as rural communities while Dagiri and Angwan shanu were selected as urban communities.
Stage 3: Using the WHO cluster sampling technique, the first house in each community was randomly selected. The center of the community was located and a bottle/pen spinned on the ground to determine the first house to participate in the study. Two houses were subsequently skipped until the number of required respondents were reached.
Stage 4: For each house, all the households were sampled. A household was defined as people eating from a common pot.
Stage 5: For household sampled with more than one eligible respondent, line list of all eligible respondent was done and one eligible respondent was randomly selected by balloting and interviewed.
NOTE: For household with no eligible respondent (women aged 25 years and above), the interviewer exited the household and sampled the immediate next available household to the right and continued the survey. The survey was continued until the sample size was achieved.
Study instrument
Primary data was collected from the respondents using a semi-structured interviewer administered questionnaire using open data kit (ODK). The questionnaire was developed based on information obtained from previous studies on breast cancer screening [
8,
9]. Data on socio demographic characteristics, knowledge on breast cancer, practice of screening and environmental/psychosocial barriers to breast cancer screening were collected. Face-to face interviews was carried out on all respondents. Eight (8) environmental factors were assessed which included long distance to health facility; poor access routes to HF; high travel cost; high cost of screening; not aware of location of screening centers; inconvenient time schedule for screening; inconvenient place for screening and long clinic waiting hours. Fourteen (14) psychosocial factors were assessed which and included; refusal from husband/spouse; not comfortable with health worker attitude; fear of being tagged promiscuous; fear of been diagnosed of cancer/its implications and stigma; unacceptable touching to my body; embarrassing to tell people about; ashamed-shy to uncover my body; fear of hospitals and health facilities; fell uneasy-distressed when come close to health care providers (HCP); previous bad experience with HCPs; busy and no time to do it; awareness program are deficient; not aware of appropriate age for screening and fear of exposure to STIs.
Data Management
After collection of data, the instrument was checked for completeness and clarity. Data collected was cleaned and consistency checks done before analysis to ensure accuracy. Data was processed using IBM Statistical Packages for Social Sciences (SPSS) Version 23. Frequency distributions, percentages, mean score, standard deviation and charts were computed and tabulated. Bivariate analysis was done using crude odd ratios at 95% CI and statistical analysis using p-value <0.05. Multivariate analysis was done using binary logistics regression at 95% CI. For each question based on knowledge, a score of one was given for a correct answer, whereas a zero score was given for incorrect and do not know responses. Questions on the knowledge part was rated and a total score obtained. The mean knowledge scores were then computed. Those with a total score below the mean were classified as having poor knowledge, whereas those with score equal to and above the mean were considered having good knowledge.
Ethical Consideration
Ethical clearance was obtained from FCT Health Research Ethics Committee (Approval Number: FHREC/2020/01/08/10-02-20). Verbal informed consent was sought and obtained from each respondent before administration of the questionnaire. Ethical issues like confidentiality, opportunity to decline interview at any stage and non-exposure to risk was also discussed with each respondent. Participation in the study was voluntary. To ensure confidentiality of information, questionnaires were filled anonymously.
Results


Five hundred and seventeen (517) research instruments were administered and five hundred and fourteen were retrieved from respondents, giving a response rate of 99.4%. The mean age of respondents was 38.36±11.6years. While 179 (34.8%) of the respondents were between ages 21-30, 174 (33.9%) were above 40 years of age. A greater percentage of the respondents 340 (66.1%) were married with 360 (70.0%) having a monogamous family type and 385 (74.9%) had between 2-3 children. About 2.1% of the respondents were not married but were staying with either their fiancés or boyfriend. 173 (33.7%) had secondary education attainments while 82 (16%) had no formal education. 38.5% of the respondents had spouses with secondary education as highest educational qualification while 7.2% of their husbands had no formal education. More than half 300 (58.4%) were Christians and 258 (50.2%) resided in rural communities Table 1.
Findings showed that 296 (57.6%) were aware of breast cancer. Their major source of information was hospital and the media while conferences/seminar was the least source of information. The main breast cancer screening method known by respondents was breast self-examination 192 (37.4%) while 316 (61.5%) were not aware of any breast cancer screening method. Respondents´ knowledge on risk factors and signs and symptoms were also assessed and result showed that 275 (53.5%) of the respondents had good knowledge while 239 (46.5%) had poor knowledge about breast cancer. Only about 73(14%) of respondent knew that overweight, lack of exercise, old age and fatty diet were risk factors for breast cancer. 344 (70%) knew that Swelling/skin irritation on all or part of the breast was a sign of breast cancer.
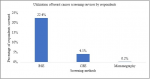
Figure 1 shows screening methods ever utilized by respondents; 115 (22.0%) of the respondents had ever done a Breast Self-Examination (BSE), 21 (4.1%) had undergone a Clinical Based Examination (CBE) while 1 (0.2%) of the respondents had utilized mammography screening method. Majority 323 (86.6%) were willing to attend a breast screening exercise and 50 (13.4%) were not willing to attend any screening. 20 (40.0%) of them said they were not willing because they don´t have time for it. Association between respondents´ willingness to screen for breast cancer with educational level, occupation and number of children were found to be statistically significant (p<0.05).
Table 2 shows the multivariate analysis using binary logistic regression to determine predictors for breast cancer screening, results showed that women who had ≥ 4 children (aOR:2.92 (95% CI: 1.601 - 5.309)) were more likely to go for screening than women who had less than 4 children.
Association between respondents´ willingness to screen for breast cancer with all environmental factors; Long distance to health facility, Poor access routes to HF, High travel cost, high cost of screening, not aware of location of screening centers, Inconvenient time schedule for screening, Inconvenient place for screening, long clinic waiting hours were found to be statistically significant (p<0.05). Multivariate analysis using binary logistic regression showed that poor access routes to health facilities (aOR:0.29 (95% CI: 0.118 - 0.701)), high cost of screening (aOR:0.29 (95% CI: 0.133 - 0.620)) and long waiting hours (aOR:0.25 (95% CI: 0.107 - 0.567)) were found to be environmental predictors of breast cancer screening
Table 3. It follows that poor access route to health facilities, high cost of screening and long waiting hours contributed to non-willingness of clients to screen for breast cancer.
Table 4 shows the bivariate and multivariate analysis using binary logistic regression to determine psychosocial predictors of breast cancer screening. At p<0.05, all psychosocial factors assessed were significant however multivariate analysis showed that fear of been diagnosed of cancer/its implications/stigma (aOR:11.41 (95% CI: 3.157 - 41.270)), fear of being tagged promiscuous (aOR:0.07 (95% CI: 0.007 - 0.810)), awareness programs are deficient (aOR:0.39 (95% CI: 0.160 - 0.960)), and not aware of appropriate age for screening (aOR:0.29 (95% CI: 0.102- 0.809), were found to be psychosocial predictors of breast cancer screening. Thus, absence of stigma, improvement in awareness programs and communication of appropriate screening age could increase screening rate.
Discussion


This research study assessed environmental and psychosocial barriers to breast cancer screening among women in Gwagwalada Area Council, FCT - Abuja. Environmental barriers to breast cancer screening include long distance to health facility, poor access route to health facilities, high cost of screening, long clinic waiting hours. Psychosocial barriers to breast cancer screening include fear of being tagged promiscuous, fear of being diagnosed of cancer awareness programs are deficient and not aware of appropriate age of screening.
The mean age of respondents was 38.36±11.6years. A larger percentage (66%) of the respondents were between 25-40 years of age, this finding is also in line with the study that states that the age specific fertility rate pattern of women in the urban settings depicts a narrow peak at age 25-29 years [
10]. In this study, majority were married and practicing monogamous family type which corresponds with the study carried out in Lagos [
11] and Saudi Arabia [
12]. Most of the respondents had secondary education as their highest level of qualification, similarly, majority of the respondents had husbands with secondary education as highest level of education, this finding is similar to the study conducted in Enugu, Nigeria [
13]. The religious groups represented were majorly Christians, this is because the FCT has different religious affiliations and the indigenes of the FCT are majorly the Gbagyi´s with majority of them practicing Christianity.
Similarly, slightly above half of the respondents had good knowledge on breast cancer including screening method, signs/symptoms and risk factors, this is similar to a study conducted in Ethiopia [
14]. It is however slightly lower than other studies reported in Lagos state Nigeria with 60% awareness rate [
15]. Variations observed in this study in comparison with other previous study may be attributed to different classes of respondents used in the study. Studies using healthcare personnel (nurses, doctors, laboratory scientists) tend to report high level of awareness.
Evidence from this study showed that Breast Self-Examination (BSE) was the most known breast cancer screening method. BSE was most practiced by majority of the respondents as compared to CBE and mammography. This is similar to findings among females attending a tertiary hospital in southwest Nigeria [
16]. The practice of BSE by most respondents as compared to other breast cancer screening method may be due to the zero cost of screening and transportation to screening site. Majority of the respondents had no reason for not undergoing the test while others attributed lack of time, old age and no interest as reasons for non-screening.
Significant environmental barriers identified by respondents to uptake of screening services include poor access routes to health facilities, high cost of screening and long clinic waiting hours. This is similar to findings from Onitsha in southeast Nigeria [
17], where about 20% of the women interviewed had never gone for screening because of inaccessibility to the screening site. Similarly, in a study carried out in Saudi Arabia [
18,
19] even though breast screening services were provided freely, utilization was low due to long waiting hour. This could also pose a challenge to women in GAC as seen from the findings as there are only seven sites that provide breast cancer screening services and only one of them is a tertiary health facility owned by the government. Client load and human resource could affect waiting time at the health facility.
Cancer screening services are mostly available in tertiary health institutions with catastrophic cost implications in most cases. High cost of screening services identified in this study as an environmental barrier to breast cancer screening is also similar with findings from an equity analysis carried out in Nigeria [
20] where cost of medical treatment was reported as a major financial barrier to the continued benefit from screening and treatment services to individuals in different social economic status groups more especially with the poorest and very poor. Economic and social factors such as poverty were directly linked with low usage of mammography screenings. Even though the present study site had a teaching hospital, uptake of services was still low. However, respondents admitted that if screening location was brought to the grass root and affordable, they would like to do the test.
The psychosocial barriers identified by respondents in this study include fear of being tagged promiscuous, fear of being diagnosed of cancer/its implications and stigma, awareness programs are deficient, not aware of appropriate age for screening. In a similar study in Spain [
21] significantly encountered barriers perceived by those never screened were stigma following the diagnosis of cancer, being busy with lack of time for screening and fear of consequences. Lack of awareness program was mentioned as a possible barrier more by women who ever screened compared to those never screened.
Findings on fear of being diagnosed of cancer/its implications and stigma, is also similar to a finding from a qualitative study in Malaysia [
22] where women mentioned that the mere mention of the word cancer often evoked fear and dread and many women did not want to discuss the topic because of certain shame if they or their relatives suffer from it. Fear of stigma has been echoed in previous study in Tanzania [
23] and strongly suggested the tendency for late presentation which had been noted among Nigerian women by several authors. Information provided on breast cancer should be directed towards benefits and not to instill fear in women.
Deficiency in awareness programs was identified as a barrier to screening and could be the reason why women were not aware of appropriate age for screening. In a study conducted among northern Nigerian [
24], lack of knowledge on breast cancer screening age and symptom accounted for 26% of reason why women do not practice screening procedure. For cancer control programs to be successful at detecting breast cancer early, especially programs that rely on women taking the initiative to seek care, community women must possess the bare minimum knowledge of breast cancer signs, symptoms and risk factors.
Fear of being tagged promiscuous is similar to other studies which showed that non uptake of screening services was due to fear of accusations of unfaithfulness and possible abandonment by partners, which is also reported as a common pattern among African women.
Strength and Limitations
The strength of this study is the inclusion of an analytical component in identifying predictors of environmental and psychosocial barriers to breast cancer screening in Gwagwalada Area Council, Federal Capital Territory, Abuja. However, there is some limitations in this study. The study was conducted in selected wards and communities in the area council therefore findings may not be entirely representative of the entire area council.
Conclusion


Screening for breast cancer among women in Gwagwalada Area Council was influenced by environmental and psychosocial factors. Environmental predictors included poor access routes to health facilities, high cost of screening and long waiting hours while psychosocial predictors included that fear of been diagnosed of cancer/its implications/stigma, fear of being tagged promiscuous, deficiency in awareness programs and not aware of appropriate age for screening.
The level of knowledge on breast cancer in this study was 47% while uptake of screening services was 22% for breast self-examination and 0.2% for mammogram. This indicates that there is need for more awareness programs to be done in this study site which can have greater effect on the study population. Health workers were identified as major source of information on cancer and as such should be continuously engaged in awareness programs to enlighten women on the diseases and the risk factors associated with it to change their wrong or negative perception about the disease. Cancer control programs should intensify campaigns and enlightenment programs to encourage all women irrespective of their educational background to participate in cancer screening. Enlightenment program should provide information on appropriate screening age, frequency of screening, signs and symptoms of cancer, risk factors, screening methods, stigma, and benefits of screening to improve the level of knowledge and uptake of screening. Integration of cancer screening programs into routine programs for women of childbearing age is also recommended to improve service uptake.
What is known about this topic
- Low uptake of breast cancer screening by women in developing countries including Nigeria;
- High cost of breast cancer screening services affects uptake of service
What this study adds
- This study showed that number of children (95% CI: 1.601 – 5.309) is a predictor that influence willingness to screen for breast cancer
- Poor access routes, high cost of screening and long waiting hours were significant environmental predictors to screening
- Fear of been diagnosed of cancer/stigma, fear of being tagged promiscuous, deficiency in awareness programs and not aware of appropriate age for screening are psychosocial predictors to screening
Competing interests


The authors declare no competing interests.
Authors' contributions


Abah Angela Ukpojo conceived, designed, and implemented the research; analyzed the results and wrote the first draft of the manuscript. Adefisoye Adewole supported with the statistical analyses and Prof Olugbenga-Bello Adenike Iyanuoluwa supervised the entire research work. All the authors gave valuable input in subsequent draft and approved the final version of the manuscript. All authors read and approved the final version of this manuscript and equally contributed to its content.
Acknowledgments


We thank the lecturers of the Department of Community Health, College of Medical Sciences, Ladoke Akintola University of Technology (LAUTECH) for supporting the review of the research work and Jommurota Community Care Initiative for providing data collectors.
Tables and figures


Table 1: Association between respondents´ socio-demographic characteristics and willingness to attend breast cancer screening among women in Gwagwalada Area Council, FCT, Nigeria - 2019
Table 2: Multivariate Analysis showing association between respondents´ socio-demographic characteristics and willingness to attend breast cancer screening
Table 3: Association between respondents´ willingness to attend breast cancer screening and environmental barriers to screening among women in Gwagwalada Area Council, FCT, Nigeria - 2019
Table 4: Association between respondents´ willingness to attend breast cancer screening and psychosocial barriers to screening among women in Gwagwalada Area Council, FCT, Nigeria - 2019
Figure 1: Utilization of breast cancer screening services by respondents among women in Gwagwalada Area Council, FCT, Nigeria - 2019
References


- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer. 2015 Mar 1; 136(5):E359-86.https://doi.org/10.1002/ijc.29210 Google Scholar
- Jeronimo J, Bansil P, Lim J, Peck R, Paul P, Amador JJ, Mirembe F, Byamugisha J, Poli UR, Satyanarayana L, Asthana S; START-UP Study Group. A multicountry evaluation of careHPV testing, visual inspection with acetic acid, and papanicolaou testing for the detection of cervical cancer. Int J Gynecol Cancer. 2014 Mar; 24(3):576-85.https://doi.org/10.1097/igc.0000000000000084 PubMed | Google Scholar
- Olasehinde O, Boutin-Foster C, Alatise OI, Adisa AO, Lawal OO, Akinkuolie AA, Adesunkanmi AK, Arije OO, Kingham TP. Developing a Breast Cancer Screening Program in Nigeria: Evaluating Current Practices, Perceptions, and Possible Barriers. J Glob Oncol. 2017 Jan 25; 3(5):490-496.https://doi.org/10.1200/jgo.2016.007641 PubMed | Google Scholar
- Jedy-Agba E, Curado MP, Ogunbiyi O, Oga E, Fabowale T, Igbinoba F, Osubor G, Otu T, Kumai H, Koechlin A, Osinubi P, Dakum P, Blattner W, Adebamowo CA. Cancer incidence in Nigeria: a report from population-based cancer registries. Cancer Epidemiol. 2012 Oct; 36(5):e271-8.https://doi.org/10.1016/j.canep.2012.04.007 PubMed | Google Scholar
- National Bureau of Statistics, Nigeria. Demographic Statistics Bulletin 2017. National Bureau of Statistics. May 2018. Accessed June 2022.
- Anne L, Eckhard K, Lonna S, Suzanne P-J, Fara M, Baba T, Dembele E, Gueye M, Bouare M, Snow C. Using Data to Improve Service Delivery: A Self-Evaluation Approach. Centre for Applied Research on Population and Development (CERPOD). May 2003. Accessed June 2022. Google Scholar
- Okunowo AA, Daramola ES, Soibi-Harry AP, Ezenwankwo FC, Kuku JO, Okunade KS, Anorlu RI. Women´s knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. Journal of Cancer Research and Practice. 2018 Feb 24; 5(3):105-111. https://doi.org/10.1016/j.jcrpr.2018.02.001 Google Scholar
- Bello TO, Olugbenga-Bello AI, Oguntola AS, Adeoti ML, Ojemakinde OM. Knowledge and Practice of Breast Cancer Screening Among Female Nurses and Lay Women in Osogbo, Nigeria. West Afr J. Med. 2011 Jul-Aug; 30(4):296-300. Google Scholar
- Madubogwu CI, Egwuonwu AO, Madubogwu NU, Njelita IA. Breast cancer screening practices amongst female tertiary health worker in Nnewi. International Journal of Cancer Research and Therapeutics. 2017 Apr-Jun; 13(2):268-275.https://doi.org/10.4103/0973-1482.188433 Google Scholar
- Adebamowo CA, Ajayi OO. Breast cancer in Nigeria. West Afr J Med. 2000 Jul 1; 19(3):179-191. Google Scholar
- O. Odusanya, Olufemi O. Tayo O. Breast Cancer Knowledge, Attitudes and Practice among Nurses in Lagos, Nigeria. Acta Oncol. 2009 Jul 9; 40(7):844-848.https://doi.org/10.1080/02841860152703472 Google Scholar
- El Bcheraoui C, Basulaiman M, Wilson S, Daoud F, Tuffaha M, AlMazroa M, Memish ZA, Saeedi MA, Mokdad AH. Breast cancer screening in Saudi Arabia: Free but almost no takers. Plos One. 2015 March 16; 10(3): e0119051.https://doi.org/10.1371/journal.pone.0119051 PubMed | Google Scholar
- Titiloye MA, Womitenren YT, Arulogun OS. Barriers to Utilization of Cervical Cancer Screening Services Among Women of Reproductive Age in Ondo, Southwest Nigeria. Afr J Biomed Res. 2017 Sep; 20:229-235. Google Scholar
- Abeje S, Seme A, Tibelt A. Factors associated with breast cancer screening awareness and practices of women in Addis Ababa, Ethiopia. BMC Women´s Health. 2019 Jan 7; 19(1):4.https://doi.org/10.1186/s12905-018-0695-9 PubMed | Google Scholar
- Odusanya OO. Breast Cancer Knowledge, Attitudes and Practices of Female School Teachers in Lagos, Nigeria. The Breast Journal. 2001 May; 7(3):171-175.https://doi.org/10.1046/j.1524-4741.1998.410062.x-i1 Google Scholar
- Olugenga_Bello AI, Oladele EA, Bello, TO, Oguntola AS. Awareness and Breast Cancer Risk Factors: Perception and screening Practices among Female in a Tertiary Institution in Southwest Nigeria. Niger Postgrad Med J. 2011 Mar; 18(1):8-15. Google Scholar
- Nwozor CM, Oragudosi AL. Awareness and Uptake of Cervical Cancer Screening among Women in Onitsha, South-East, Nigeria. Greener J Med Sci. 2013 Oct 26; 3(8):283-288.https://doi.org/10.15580/gjms.2013.8.280913864
- Abdel-Aziz SB, Amin TT, Al-Gadeeb MB, Alhassar AI, Al-Ramadan A, Al-Helal M, Bu-Mejdad M, Al-Hamad LA, Alkhalaf EH. Perceived barriers to breast cancer screening among Saudi women at primary care setting. J Prev Med Hyg. 2018 Mar 30; 59(1):E20-E29.https://doi.org/10.15167/2421-4248/jpmh2018.59.1.689 PubMed | Google Scholar
- Ibrahim EM, Zeeneldin AA, Sadiq BB, Ezzat AA. The present and the future of breast cancer burden in the Kingdom of Saudi Arabia. Med Oncol. 2008 Mar 04; 25:387-393.https://doi.org/10.1007/s12032-008-9051-5 Google Scholar
- Okoronkwo I, Ejike-Okoye P, Chinweuba A, Nwaneri A. Financial barriers to utilization of screening and treatment services for breast cancer: An equity analysis in Nigeria. Niger J Clin Pract. 2015 Mar-Apr; 18(2):287-291.https://doi.org/10.4103/1119-3077.151070 Google Scholar
- March S, Villalonga B, Sanchez-Contador C, Vidal C, Mascaro A, Bennasar ML, Esteva M. Barriers to and discourses about breast cancer prevention among immigrant women in Spain: a qualitative study. BMJ Open. 2018 Nov 18; 8(11):e021425.https://doi.org/10.1136/bmjopen-2017-021425 PubMed | Google Scholar
- Maryam A, Suzie C, Asnarulkhadi AS, Gary K, Mohammed BS. Psychosocial Predictors of Breast Self-Examination among Female Students in Malaysia: A Study to Assess the Roles of Body Image, Self-efficacy, and Perceived Barriers. Asian Pac J Cancer Prev 2016 Apr 11; 17(3):1277-1284. https://doi.org/10.7314/APJCP.2016.17.3.1277 Google Scholar
- Chao CA, Huang L, Visvanathan K, Mwakatobe K, Masalu N, Rositch AF. Understanding women's perspectives on breast cancer is essential for cancer control: knowledge, risk awareness, and care-seeking in Mwanza, Tanzania. BMC Public Health. 2020 Jun 15; 20(1):930.https://doi.org/10.1186/s12889-020-09010-y PubMed | Google Scholar
- Azubuike SO, Celestina UO. Breast Cancer: The Perspective of Northern Nigerian Women. Int J Prev Med. 2015 Dec 28; 6:130. https://doi.org/10.4103/2008-7802.172803 PubMed | Google Scholar