Descriptive Characterization of Suspected Yellow Fever Cases in Kano state, Nigeria, 2015-2018
Usman Yahya Umar1,2,&, Kabiru Sabitu3, Shehu Sani Mohammed3, Nura Yahya Karaye4, Muhammad Shakir Balogun2
1Aminu Kano Teaching Hospital, Kano, Nigeria, 2Nigeria Field Epidemiology and Laboratory Training Program, Abuja, Nigeria, 3Ahmadu Bello University Zaria, Nigeria, 4Ministry of Health Kano State, Kano, Nigeria
&Corresponding author
Usman Yahya Umar, Aminu Kano Teaching Hospital, Kano, Nigeria. Email: uthmanumar1079@gmail.com
Introduction:
Yellow fever remains a serious public health problem globally with an estimated
200, 000 cases annually despite the availability of an effective vaccine for more than 70 years. Nigeria had an outbreak of Yellow fever in 2017 after more than 2 decades of silence. We described the epidemiological characteristic of yellow fever in Kano State from 2015 to 2018.
Methods:
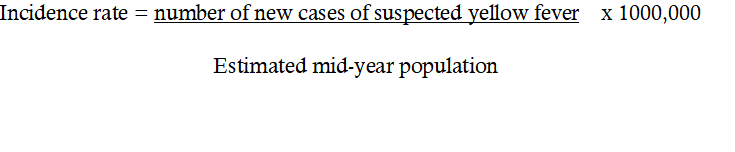
We conducted a retrospective review of suspected cases of yellow fever in Kano state from January 2015 to December 2018. A suspected yellow fever case was defined as any person residing in Kano state with sudden onset of fever, with jaundice appearing within two weeks of the onset of the first symptoms from the year 2015 to 2018. We calculated incidences, frequencies and proportions using Microsoft excel 2016 and health mapper version 4.3.
Results:
A total of 107 patients with suspected yellow fever were reported in the state between 2015 and 2018. The median age of the suspected cases was 13years (range 2-120years) and age group 15-44years had the highest number of cases. More males were affected 69 (64%) with rural local governments having the highest number of patients. Generally, the disease occurred all year round with peaks occurring the wet season mostly in June, July and August. The annual incidence increased from 1.7/1,000,000 populations in 2015 to 2.2/1,000,000 populations in 2016, remained at 2.2/1,000,000 populations in 2017 and slightly decreased to 2.1/1000,000 population in 2018. No mortality was recorded during the reporting period. Majority (99.1%) of the suspected patients had never received yellow fever vaccine.
Conclusion:
The study revealed no change in the incidence rate of suspected Yellow Fever cases in Kano State. Majority of the suspected cases are in the rural areas where immunization coverage was very low. Routine immunization has to be strengthened to address the problem. The findings were reported to the Kano state Ministry of Health for appropriate action.
Introduction

Globally, thousands of people are infected with yellow fever and majority of them die due to failure to be immunized. Serious outbreaks were documented in North and South America, Africa and Europe. In the United States and Europe, the cases were mostly travelers who got the disease from areas with high rate of transmission [1]. It is estimated that annually about 200,000 people are infected, of which about 30, 000 die. Yellow fever is a mosquito-borne flavivirus disease which is endemic in tropical South America and Sub-Saharan Africa. Yellow fever virus is transmitted by mosquitoes´ bites (Aedes and Haemogogus species) and has three cycles of transmission, namely, jungle (sylvatic), intermediate (savannah) and urban. The sylvatic cycle occurs in the forest among non-human primates that serve as primary reservoirs of the virus. The urban cycle on the other hand, is initiated when an infected person brings the virus into densely populated areas with low vaccine coverage. While the intermediate cycle involves transmission of the virus from mosquitoes to humans living in areas bordering forest zones.[1,2] The mosquito vector is prevalent in many states of Nigeria. In major cities, most people use containers to store water for domestic purposes. These containers can serve as a breeding site for the Aedes aegypti mosquito. Similarly, other artificial breeding site like tyres, cans and old vehicles may exist because of inadequate waste management especially in the urban slums. In the villages, farming activities including irrigation farming can provide favourable habitat for the vector.[3]
The manifestations of Yellow fever disease may include sudden onset of fever, relative bradycardia, and severe headache. Sometimes it can be severe, where it can manifest with jaundice, hemorrhage, and multiorgan failure. Most people with initial symptoms improve within a week. A few people will develop a more severe form of the disease. Among those who develop severe disease, mortality rate can be high with death rates of 30-60%. There is no definitive antiviral treatment for yellow fever. Vaccination is the only preventive and effective measure against yellow fever infection. A single dose of the vaccine is adequate to give lifelong protection against the disease.[
2-4] Other control strategies include efficient surveillance, effective and robust outbreak response, high-coverage vaccination, good management of cases and vector management.[
2]
In Africa it was estimated that over 500 million people are at risk of yellow fever infection and higher percentage of outbreaks (90%) occur in the region, all ages are susceptible and the infection to case ratio can range from 20:1 to 2:1 [
5,
6]. Outbreaks have been documented in Angola, Democratic republic of Congo, Uganda, Kenya, Sudan, Cameroon, Chad, Senegal, Sierra Leone and Nigeria among others. The outbreak in Angola began in December 2015 and has decimated not less than 355 persons. The outbreak later spread to the neighbouring countries of Democratic republic of Congo, Kenya and Uganda. Furthermore, between 2005 and 2016, Sudan witnessed three outbreaks with 1,508 cases reported and 368 deaths documented. [
6,
7] WHO have identified twelve countries in Africa, including Nigeria that are at high risk of yellow fever outbreaks. This is due to large non-immune individuals, as such, strengthening of routine immunization as well as preventive vaccination campaigns is crucial in these countries.[
2]
In Nigeria, after 21 years of silence, the country recorded its first confirmed case of yellow fever in Ifelodun local government of Kwara state further investigation has led to discovery of 55 suspected cases.[
2] As of December 2018, 3,902 suspected cases of yellow fever were reported from 580 local government areas (LGAs) in the country. The Pasteur institute Dakar (IP Dakar) confirmed 78 cases which were from 14 states including Kano. Total deaths reported were 73, giving a case fatality rate of 1.9%.[
8] Sub-optimal uptake of yellow fever vaccination coverage may have contributed to the outbreaks in various parts of the country. This is evident in results of immunization coverage surveys conducted in the country, where coverage of 41%, 41%,39% and 69% were obtained in 2015, 2016, 2017 and 2018 respectively for yellow fever vaccination.[
4] These values are lower than the 80% minimum cut-off value for herd-immunity.[
2] Kano State was selected for this study due to preponderance of mosquito vectors of the disease and also occurrence of confirmed yellow fever outbreak in the state between January to February, 2018. In the same vein, the immunization coverage figures for yellow fever in the state are almost similar to the national values, which are lower than the minimum 80%. In the 2016/2017 multiple indicator cluster survey/national immunization coverage survey, yellow fever coverage of 22.3% was obtained in Kano state.
Although data on suspected yellow fever are captured in Kano state epidemiologic database, the data have not been analyzed and published. The limited information and epidemiologic data on burden of yellow fever may cloud the understanding needed to put in place public health policies for appropriate intervention. We determine the trend of suspected yellow fever cases and characterized the burden of from 2015 to 2018 in Kano state using data from the state epidemiologic database to inform interventions.
Methods


Study Area
Kano state is located in the North-western part of Nigeria. It is bordered by Jigawa state to the North-East, Bauchi to the South-East, Kaduna to the South-West and Katsina to the North-west. The estimated population of the state is over 13 million from 2006 census and it has 44 local government areas.[
5] The main inhabitants of the state are Hausa-fulanis who are predominantly Muslims, there are also Nigerians from other parts of the country, notable among them are the Yorubas, Igbos and Kanuris. Hausa is the main language spoken among the inhabitants, while English is the official language. The main occupation among the people in the state is farming, a significant proportion of the people in the state are engage in different businesses while others are civil servants. The state is located between Latitude 13°W and 11°S and Longitude 8°W and 10°E. The temperature ranges between 15.8°C to 33°C but it may be as low as 10°C during the cold season. The state has two seasonal periods; dry season which extends from October to April and rainy season that extends from May to September with an average rainfall of 63.3mm±48.2 and 133,4mm±5
9mm respectively. The climatic condition together with the abundant agro-ecological habitats found in most local government areas in the state provide a conducive atmosphere for the breeding of the mosquito vectors and yellow fever transmission. In total, Kano state has 1374 health facilities, 1223 are public owned while 151 are private facilities.
Study population
The study was conducted among all suspected yellow fever cases from the local government areas reporting priority diseases to the state epidemiology unit in the state ministry of health irrespective of their age and sex from 2015-2018.
Study design
In a cross sectional study, we reviewed secondary data from the Kano state yellow fever surveillance system. The data had been generated through health facility and house to house active case search whenever there was a report of suspected yellow fever case in any of the local government areas of the state. The rapid response team undertake an advocacy visit to the community leaders of the affected area prior to the response activities to create awareness among the community members on the nature and the risk associated with the disease. The visit also facilitates smooth engagement with house-holds through their heads. House-hold members were asked for history of fever and jaundice. Those cases that met the standard case definition were included in a line-list. Respondents that had relevant signs and symptoms which had resolved or could not be verified were excluded from the line-list.
Data Source
Data was retrieved from the IDSR yellow fever line list form 001C, fully completed case investigation forms The data consist of recovered from the 44 local governments public and private health facilities across Kano state spanning January to December of the years 2015, 2016, 2017 and 2018.
Case Definitions
Suspected yellow fever case: Any person living in Kano state with sudden onset of fever and jaundice within two weeks of the onset of the first symptoms from the year 2015 to 2018 [
9].
Statistical Analysis
The data was analyzed using the Microsoft Excel 16.0 (Microsoft Corporation, One Microsoft Way, Redmond, USA) and health mapper version 4.3. Incidence rates, frequencies and proportions were calculated for the cases and presented in tables and charts and map. For calculation of incidence rate, the formula below is used
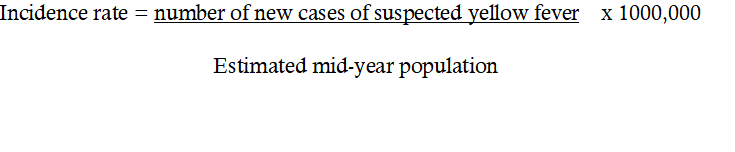
For the year 2015, there were 21 cases of suspected yellow fever and the estimated population = 12,568,291, therefore the incidence rate =
21/12,568,291 x 1000,000 = 1.7 per million population
For the year 2016, with 28 new suspected cases and estimated population of 12,983,043, the incidence rate = 2.2 per million population
For the year 2017, there were 29 new suspected cases and the estimated population was 13,411,483, the incidence rate = 2.2 per million population
Lastly, in 2018, there were 29 cases and the estimated population was 13,951,499 giving an incidence rate of 2.1 per million population.
Ethical consideration
Approval was obtained from the state Ministry of health with a reference number MOH/OFF/797/T.1/1142 dated 1
stFebruary 2019. The personal identifying information on the data were removed to ensure that the confidentiality of the involved was maintained. The data were only made available to the relevant members of the team for the purpose of analysis and data interpretation only and were stored in password protected computer systems.
Results


We investigated the magnitude and trend of yellow fever in Kano state and found out that significant number of suspected cases reported across all ages and sexes during the reviewed period. The study revealed a total of 107 patients with suspected yellow fever reported in the state between 2015 and 2018. The median age of the suspected cases was 13years (range 2120years) and age group 15-44years had the highest number of cases. Majority of the suspected case (99.1%) had never received yellow fever vaccine (Table 1). Result also demonstrated that males were more affected 69 (64%) (Table 1), with rural or relatively agrarian local governments areas having the highest number of the suspected cases (Figure 1). No mortality was recorded during the reporting period (Table 2). The disease occurred all year round with peaks occurring during wet season mostly in June, July and August (Figure 2). The annual incidence increased from 1.7/1,000,000 populations in 2015 to 2.2/1,000,000 populations in 2016, remained at 2.2/1000,000 population in 2017 and slightly decreased to 2.1/1,000,000 populations in 2018 (Figure 2).
Discussion


The incidence of the suspected yellow fever had remained relatively stable over the review period with some male preponderance. This could be due the fact that male tend to be highly mobile during the day time especially in the rural areas, engaged in activities like farming, hunting, mining and animal rearing which may expose them more to mosquito vectors of the disease.[10,11] This is similar to the findings of Goldani in Brazil, who found that majority of the cases of yellow fever tend to occur among males in the population especially among those in the rural areas and in the active segment of the population.[12] More so, Lilay et al in Ethiopia found a slightly more male preponderance compared to female.[11] However, Babaniyi et al in Zambia found no sex difference.[1] The study also found out that the most affected age group were 15-44 years followed by 5-14 and 0-4years in that order, while age group ≥45 seemed to be the least affected. The 15-44years are the active segment of the population that is also involve in agrarian and other activities that may predispose them to the disease. The finding of significant number of the suspected cases among the age groups 0-4 and 5-14 reflected the gap in routine immunization services and also the fact that most African countries including Nigeria have dropped mass yellow fever vaccine campaign [13,14]. In a study by Cassey et al in the United States, it has been shown that children even when vaccinated have lower seroconversion rate when compared with adults. As such they have higher tendency to come down with the disease [15].
Cases were recorded all year round with some variations, but the highest peaks were recorded during the wet season (May to September), which is characterized by high amount of rain showers that encourage the breeding of the mosquitoes [16,17.] Bagwai and Shanono local governments recorded the highest number of cases followed by Karaye. Areas in rural settings may have vegetation which may serve as an excellent breeding sites for the Aedes mosquitoes, and people living in these places tend to be more exposed to the bite of the mosquitoes. Studies by Kaul et al in Brazil have corroborated these findings, where they found out that majority of the cases occurred during the wet season as the vectors occur in abundances during this period [18]. Similarly, Agha et al in Kenya have documented that the vectors for the yellow fever were highest during the long rains compared to any other period [19]. Equally, small-scale epidemics are more likely due to the peri-domestic mosquitoes that can bite both humans and wild animals [20].
The vaccination status among the suspected cases was approximately 1%, majority of them were not vaccinated. Data obtained from district health information (DHIS2) showed that Bagwai LGA had good yellow fever immunization coverages of 91.7%, 93.1% and 89.2% in 2015, 2016 and 2017 respectively. However, in 2018, a coverage of 74,2% was obtained, which is below the WHO recommendation. Despite the good coverage recorded in the first three years of the study, a sizeable number of suspected cases were observed. This may be explained by the fact that DHIS2 data is mainly generated from routine immunization activities which do not include coverage for other age groups. In the endemic regions like Nigeria, immunologic response to yellow fever vaccination may have to be interpreted in the context of confounding factors like parasitic infestation, anaemia and malnutrition.[
6] On the other hand, DHIS2 data for Shanono local government area showed a sub-optimal coverages of 57.7%, 70.7%, 59.4% and 73.6% for 2015, 2016, 2017 and 2018 respectively.[
7] These values clearly depict a large gap in yellow fever vaccination in the affected local government. Therefore, there is high likelihood of low coverage levels in the local government areas with high number of suspected of yellow fever cases. A study by Saad et al showed that most cases of yellow fever infection occurred in unvaccinated individuals and no infections were seen among the individuals who were vaccinated [
21]. In the same vein, a study by Butler has shown that some African countries like Nigeria have less than 50% immunization coverage for yellow fever. These low coverage levels may have contributed in the accumulation of high number of susceptible individuals that can serve as a trigger for outbreaks at any time.[
8] The availability of the vaccines has led underestimation of the threat posed by the disease.[
22] In Nigeria, apart from the low vaccination coverage, other factors that may have contributed to the high burden of yellow fever in the country include large population size and moderately high infection forces [
8].
Finally, there were no mortalities recorded. This is possible because in majority of the individuals infected, the disease tends to be mild and self-limiting. Also, majority of the cases detected were young adults that are likely to be healthier. On the other hand, it may be possible for the patient to have a severe form of the disease and have a bad prognosis at the end or even die but it may not be captured in the state line list due to limited follow up [
2,
23].
Limitations of the study include underreporting and possibly non-reporting by some local government areas in the state. Also, some of the cases do not have confirmatory laboratory results. Moreover, there was very limited clinical information documented in the line-list, as such appropriate categorization of the patients cannot be done.
Conclusion


The number of suspected cases of yellow fever continued to increase annually in Kano. Male population and the age group 15-45 seemed to be the mostly affected. Bagwai and Shanono local government areas which are located in the rural areas have the highest number of suspected cases. Transmission occurs all year round with the highest peak in wet season. Low level of immunization among children also contributes significantly to the re-emergence of the disease. The outcome was generally good as no mortality was recorded among the reported cases.
We recommended strengthening routine immunization and mass vaccination campaign especially in the rural areas. Laboratory confirmation of the surveillance should be improved to make the system better. Equally, the clinical components should be included in the line-list to help in the categorization of the patients.
Acknowledgments


We acknowledged the assistance given to us by Ministry of health Kano state especially the epidemiology unit in acquiring the data for this study. We are very grateful. We acknowledge the support of Dr Chukwuma Umeokonkwo in reviewing the draft manuscript and providing support in interpretation of the data analysis.
Competing Interest


The authors declare that they have no competing interests.
Authors' contributions


UYU conceptualized the study, designed, implemented data acquisition, drafted the initial manuscript and data analysis. KS made substantial revision of the initial manuscript. SSM supervised the study and made substantial revision of the initial manuscript. NYK implemented data acquisition and made substantial addition to the initial manuscript. MSB made substantial revision of the draft manuscript. All authors read and approved the final manuscript.
What is already known on this topic?


- Yellow fever is a viral hemorrhagic fever that remains a serious public health problem globally
- About 200,000 cases are reported annually despite the availability of an effective vaccine for more than seven decades
- Nigeria started having yellow fever outbreaks in 2017 after more than two decades of silence
What this study adds


- The study adds information on the incidence rate of suspected yellow fever in Kano state and report on a four-year trend analysis of suspected yellow fever cases in Kano state.
- The study used surveillance data to estimate the trends and rates. This shows the significance of using routinely collected data to inform public health interventions and also to improve the data collection systems
- Re-emergence of yellow fever in kano state is partly due to gaps in yellow fever vaccination
Tables and Figures


Table 1: Demographic characteristics of yellow fever cases in Kano state 2015-2018
Table 2: Management modalities and outcome among the suspected yellow fever cases in Kano state from 2015-2018
Figure 1: Cumulative distribution of suspected yellow fever cases by LGAs in Kano state 2015-2018
Figure 2: Trend of suspected Yellow fever cases in Kano state over the four-year period 2015-2018
References


- Babaniyi O, Chizema E, Eshetu-Shibeshi M, Malama C, Masaninga F, Mazaba-Liwewe M, Monze M, Mulenga D, Mwaba P, Mweene-Ndumba I, Rudatsikira E, Siziya S, Songolo P. Risk assessment for yellow fever in western and North-Western provinces of Zambia. J Global Infect Dis. 2015;7(1):1 https://doi.org/10.4103/0974-777x.150884. PubMed | Google Scholar
- Yellow fever [Internet]. CDC; 2019 [cited 2021 Jan 11].<
- Yellow fever: [Internet]. WHO. World Health Organization; [cited 2021 Jan 11].
- Brooks GF, Jawetz E. Jawetz, Melnick, & Adelberg´s medical microbiology. 26. ed. New York: McGraw-Hill Medical; 2013. 864 p. (A Lange medical book). | Google Scholar
- WHO | Yellow fever - Nigeria [Internet]. WHO. World Health Organization; [cited 2021 Jan 11].
- Lucey D, Gostin LO. A yellow fever epidemic: a new global health emergency? JAMA. 2016 Jun 28;315(24):2661. https://doi.org/10.1001/jama.2016606. PubMed | Google Scholar
- Grobbelaar AA, Weyer J, Moolla N, Jansen van Vuren P, Moises F, Paweska JT. Resurgence of yellow fever in angola, 2015-2016. Emerg Infect Dis. 2016 Oct;22(10):1854-5. https://dx.doi.org/10.3201/eid2210.160818.. PubMed | Google Scholar
- Weekly Epidemiological Report-Abuja, December 2018 [Internet]. Nigeria Centre for Disease Control. Nigeria Centre for Disease Control; 2018 [cited 2021 Jan 11]. Available from: https://ncdc.gov.ng/reports/164/2018-december-week-49.
- WHO | Yellow fever situation report [Internet]. WHO. World Health Organization; [cited 2021 Jan 11].
- Alhakimi HA, Mohamed OG, Khogaly HSE, Arafa KAO, Ahmed WA. Epidemiological, clinical and entomological characteristics of yellow fever outbreak in darfur 2012. AIMS Public Health. 2015;2(1):132-41. https://dx.doi.org/3934%2Fpublichealth.2015.1.132. PubMed | Google Scholar
- Lilay A, Asamene N, Bekele A, Mengesha M, Wendabeku M, Tareke I, Girmay A, Wuletaw Y, Adossa A, Ba Y, Sall A, Jima D, Mengesha D. Reemergence of yellow fever in Ethiopia after 50 years, 2013: epidemiological and entomological investigations. BMC Infect Dis. 2017 Dec;17(1):343. https://doi.org/10.1186/s12879-017-2435-4. PubMed | Google Scholar
- Goldani LZ. Yellow fever outbreak in Brazil, 2017. The Brazilian Journal of Infectious Diseases. 2017 Mar;21(2):123-4. http://dx.doi.org/10.1016/j.bjid.2017.02.004. PubMed | Google Scholar
- Shearer FM, Moyes CL, Pigott DM, Brady OJ, Marinho F, Deshpande A, Longbottom J, Browne AJ, Kraemer MUG, O´Reilly KM, Hombach J, Yactayo S, de Araújo VEM, da Nóbrega AA, Mosser JF, Stanaway JD, Lim SS, Hay SI, Golding N, Reiner RC. Global yellow fever vaccination coverage from 1970 to 2016: an adjusted retrospective analysis. The Lancet Infectious Diseases. 2017 Nov;17(11):1209-17. https://doi.org/10.1016/s1473-3099(17)30419-x. PubMed | Google Scholar
- Rogers DJ, Wilson AJ, Hay SI, Graham AJ. The global distribution of yellow fever and dengue. In: Advances in Parasitology [Internet]. Elsevier; 2006 [cited 2021 Jan 11]. p. 181-220. https://dx.doi.org/10.1016%2FS0065-308X(05)62006-4. PubMed | Google Scholar
- Casey RM, Harris JB, Ahuka-Mundeke S, Dixon MG, Kizito GM, Nsele PM, Umutesi G, Laven J, Kosoy O, Paluku G, Gueye AS, Hyde TB, Ewetola R, Sheria GKM, Muyembe-Tamfum J-J, Staples JE. Immunogenicity of fractional-dose vaccine during a yellow fever outbreak – final report. N Engl J Med. 2019 Aug 1;381(5):444-54. https://doi.org/10.1056/nejmoa1710430. PubMed | Google Scholar
- Hamrick PN, Aldighieri S, Machado G, Leonel DG, Vilca LM, Uriona S, Schneider MC. Geographic patterns and environmental factors associated with human yellow fever presence in the Americas. Barker CM, editor. PLoS Negl Trop Dis. 2017 Sep 8;11(9):e0005897. https://doi.org/10.1371/journal.pntd.0005897. PubMed | Google Scholar
- Barnett ED. Yellow fever: epidemiology and prevention. Clinical Infectious Diseases. 2007 Mar 15;44(6):850-6. https://doi.org/10.1086/511869. PubMed | Google Scholar
- Kaul RB, Evans MV, Murdock CC, Drake JM. Spatio-temporal spillover risk of yellow fever in Brazil. Parasites Vectors. 2018 Dec;11(1):488. https://doi.org/10.1186/s13071-018-3063-6. PubMed | Google Scholar
- Agha SB, Tchouassi DP, Bastos ADS, Sang R. Dengue and yellow fever virus vectors: seasonal abundance, diversity and resting preferences in three Kenyan cities. Parasites Vectors. 2017 Dec;10(1):628. https://doi.org/10.1186/s13071-017-2598-2. PubMed | Google Scholar
- Ribeiro Leite Jardim Cavalcante K, Luiz Tauil P. Características epidemiológicas da febre amarela no Brasil, 2000-2012. Epidemiol Serv Saúde. 2016 Jan;25(1):10-1. http://dx.doi.org/10.5123/S1679-49742016000100002. PubMed | Google Scholar
- Saad LDC, Barata RB, Saad LDC, Barata RB. Surtos de febre amarela no estado de São Paulo, 2000-2010*. Epidemiologia e Serviços de Saúde. 2016 Sep;25(3):531-40. https://doi.org/10.5123/s1679-49742016000300009. PubMed | Google Scholar
- Butler D. Fears rise over yellow fever´s next move. Nature. 2016 Apr;532(7598):155-6. https://doi.org/10.1038/532155a . PubMed | Google Scholar
- Kallas EG, D´Elia Zanella LGFAB, Moreira CHV, Buccheri R, Diniz GBF, Castiñeiras ACP, Costa PR, Dias JZC, Marmorato MP, Song ATW, Maestri A, Borges IC, Joelsons D, Cerqueira NB, Santiago e Souza NC, Morales Claro I, Sabino EC, Levi JE, Avelino-Silva VI, Ho Y-L. Predictors of mortality in patients with yellow fever: an observational cohort study. The Lancet Infectious Diseases. 2019 Jul;19(7):750-8. https://doi.org/10.1016/S1473-3099(19)30125-2. PubMed | Google Scholar