Perinatal Mortality in Emergency Obstetric Health Care Facilities, Nakuru County, Kenya, 2014-2017: A descriptive cross sectional surveillance data analysis
Ben Kipchumba Ngare1,&, Yuster Ronoh2, Maurice Owiny1,3, Caren Gesare1, Zeinab Gura1
1Kenya Field Epidemiology and Laboratory Program-Kenya, 2Nakuru County Department of Health Services, Kenya, 3African Field Epidemiology Network
&Corresponding author
Ben Kipchumba Ngare, Kenya Field Epidemiology and Laboratory Training Program-Nairobi, Kenya. kipchumba.ben@gmail.com
Introduction:
Perinatal mortality is a major global public health problem. In 2016, 2.6 million perinatal deaths were reported globally, in Kenya, it accounted for 22.6 deaths/1000 live births. We sought to describe perinatal mortality in Nakuru County.
Methods:
We reviewed “perinatal mortality” on System data report between 2014–2017. Perinatal death was defined as any record of death in the first seven days of life and stillbirths that occurred in health facilities that provided emergency obstetric care. We assessed age, time and place of death occurrence, neonatal and maternal clinical characteristics. We calculated the perinatal mortality rate (PNMR), trends, frequencies and proportions for characteristics of interest.
Results:
A total of 59,152 births were reported in 9 facilities from 2014–2017, 929 of these births were subsequently classified as perinatal deaths. Overall PNMR was 15 deaths/1000 live births.
Among those who died their mean age was 0.83±0.05 day. Early neonatal deaths: 533(57.6%), Stillbirths: 382(41.0%) and 14(1.4%) cause of deaths were not recorded. Nakuru Level-5 Hospital recorded 835(90%) perinatal 15 deaths. In 2014, PNMR was 25.1 deaths/1000 live births which reduced to 12.5 deaths/1000 live births in 2017. Of the infants who died 570(61.4%) were <1 day old. Partograph was not used in 464(49.9%) of the pregnant women. Reported contributors of perinatal deaths were birth asphyxia 275(29.6%), prematurity 267(28.7%) and low-birth-weight 252(27.1%).
Conclusion:
Nakuru County PNMR was higher compared to WHO recommendation of < 12 deaths/1000 live births, therefore, there is need to identify strategies to reduce incidences of asphyxia, prematurity and low birth weight. Comprehensive antenatal coverage, adequate care of infants at birth is likely to improve quality of life among the survivors and reduce PNMR.
Introduction

Perinatal mortality is a major public health problem in many low and middle income countries (LMICs). The world health organization (WHO) defines perinatal mortality as either a stillbirth after at least 22 completed gestational weeks, or an early neonatal death in the first 7 days after birth[1] . It has been reported to be associated with inadequate access to quality care services [2] and, suboptimal environmental conditions [3]. Almost half of the stillbirth and early neonatal mortality occurs during the period of labor and delivery (4); with prematurity, low birth weight, obstructed labor, pregnancy complications, infections and birth asphyxia were identified as the leading causes for these untimely deaths [5-7].
Globally, approximately, 2.6 million newborns died in 2016 translating to 7000 neonatal deaths per day, These deaths have been increasing from 41% in 2000 to 46% in 2016 of all under-five deaths [
8].
About 95% of these deaths occurred in LMICs with the largest numbers reported in South Asia and Sub-Saharan Africa [
8] Perinatal mortality remains an urgent public health concern and progress made has been slower than that reported for maternal and child mortality [
9-11].
In Sub Saharan Africa, current perinatal mortality accounts for 40% of all global deaths among under 5 years old and, 76 per 1000 live births dies within the first 7 days of life. Of 79 countries with above 25% under 5 mortality rate 35 countries are from Sub Saharan Africa [
12]. This hinders the progress towards the achievement of the proposed Sustainable Development Goal (SDG) target 3.2 which aims at ensuring healthy lives of children and promoting their wellbeing and reduction of under 5 year mortality to less than 25/1000 by 2030 [
13,
14].
In Kenya, perinatal mortality is 22.6 /1000 live births; this is still high and has remained a major problem despite of the free maternity services. This was an increase compared to an average Neonatal mortality of 15 deaths per 1000 live births according to a study report done between 2011 and 2015 [
15].
In Nakuru County, little is known regarding perinatal mortality, therefore, we sought to describe perinatal mortality from 2014-2017.
Methods


Study site
The study site was Nakuru County. It has 11 Sub-counties with an estimated population of 1,873,174 people. The number of women of reproductive age is 433,167, the annual projected deliveries are 79,722 and the approximated number of under 1-year children is 63,688.
It has 166 public health facilities out of which 9 offer emergency and obstetric services, 155 Faith-Based Organization, and 189 Private Health facilities.
In Nakuru County, Perinatal death data is captured using Perinatal Maternal Death Surveillance Report Form (PMDSR) by facility in-charge at the facility level, then submitted to the Sub County Health Records and Information Officer (SCHRIO) for uploading to the National Health Information System-Kenya Health Information System (KHIS).
Study Design
We reviewed of perinatal mortality data reported in the KHIS from January 2014 and December 2017, population included reported cases of >22 gestational weeks in the KHIS.
Case definition
We defined a perinatal death as any record of death in the first seven days of life and stillbirths after at least 22 completed gestational weeks that occurred in health facilities that provide emergency obstetric care in Nakuru County between January 2014 and December 2017.
Inclusion criteria
Any record of death in the first seven days of life and stillbirths after at least 22 completed gestational weeks that occurred in health facilities that provide emergency obstetric care in the KHIS for Nakuru County between January 2014 and December 2017.
Exclusion criteria
Any record of fetal death of less than 22 gestational weeks and >7 days after birth in KHIS for Nakuru County between January 2014 and December 2017.
Definition of terms according to the World Health Organization
Perinatal Mortality Rate (PNMR) -is the number of stillbirths and deaths in the first week of life per 1,000 total births.
Still birth-refers to a dead born fetus.
Early Neonatal death-refers to deaths occurring during the first one week after birth.
Live birth is the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which, after such separation, breathes or shows any other evidence of life, such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles, whether or not the umbilical cord has been cut or the placenta is attached.
Data collection
We abstracted perinatal mortality data from KHIS between January 2014 and December 2017 and the variables on age, time, place, Partograph use, neonatal and maternal characteristics were abstracted.
Data management
The abstracted data was cleaned using Microsoft Excel 2013 (Microsoft Office, Seattle, USA), and analyzed using Epi-Info 7.2.2TM. (CDC-Atlanta).
Perinatal Mortality Rate (PNMR) was calculated by summing up of all fetal deaths after 22 or more weeks of gestation (stillbirths) and deaths of infants less than 7 days of age then divided by the sum of the of all live births and fetal deaths after 22 or more weeks of gestation (stillbirths) and then multiplied by 1000 live births in the 9 Emergency Obstetric Health Care Facilities in Nakuru County, Kenya from 2014-2017.
We performed the summary descriptive statistics in data analysis in Microsoft excel to calculate the measures of central tendency and dispersion (mean age and standard diversion.
We calculated counts, frequencies, proportions for categorical variables.
Analyzed data was presented in tables and graphs.
We used Quantum geographic information system (QGIS) version 2.18.2 (Gary Sherman, USA) to draw and illustrate the distribution of emergency obstetric facilities with their respective PNMR in Nakuru County; we got the facility GPS co-ordinates from the Kenya e-health facilities list, these co-ordinates were fed into the QGIS to plot spot map of these facilities.
Permission to access Nakuru KHIS Perinatal Mortality Data
Permission was sought from Nakuru County Department of Health Services to access their KHIS data and we used password protected computers to maintain the utmost confidentiality of the collected information.
Results


Descriptive statistics Results
From 2014-2017, a total of 59,152 births were reported in the 9 Emergency and Obstetric health care facilities, 929 of these births were subsequently classified as perinatal deaths. The overall Perinatal Mortality Rate (PNMR) was 15 deaths per 1000 live births. The mean age among those who died was 0.83±0.05 day.
Early neonatal deaths were 533 (58%), Stillbirths were 382 (41.6 %), and while 14 (1.4%) causes of deaths were not recorded. Nakuru Level 5 Hospital recorded 835 (90%) Perinatal deaths N=929 with PNMR of 23.4/1000 live births, this was followed by Nakuru Annex Hospital with 55(5.7%) with PNMR of 2.7/1000 live births
Table 1 and the distribution of Emergency Obstetric Health care facilities with respective perinatal mortality rate in Nakuru County are shown by
Figure 1.
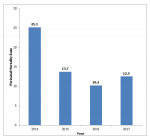
In 2014, PNMR was 25.1 deaths per 1000 live births, this declined to 13.7 deaths per 1000 live births in 2015 and further declined to 10.2 deaths per 1000 live births in 2016, in 2017, PNMR slightly rose to 12.5 deaths per 1000 live births
Figure 2.
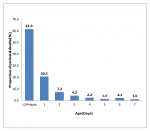
Five hundred and seventy (61.4%) of the infants who died were under one day old
Figure 3.
Partograph was not used in 464(49.9%) of the pregnant women
Table 2.
Reported contributors of perinatal mortality in Nakuru County, 2014-2017
Among the infants who died 275(29.6%) had birth asphyxia, this was followed with those who were premature 267(28.7%), then those who had low birth weight 252(27.1%) and those who suffered hypothermia were 38(4.1%)
Table 3.
Discussion


The study found out that: the overall PNMR in Nakuru was lower than National PNMR of 22 perinatal deaths per 1000 live births.
Infants who had birth asphyxia accounted for one third of the perinatal deaths this was in agreement with a study Maternal and Newborn Health Disparities in Kenya [
14] and more than half of the perinatal mortality consisted of early neonatal deaths similar to the findings on Perinatal Mortality Magnitude, Determinants and Causes in West Gojam a Population-Based Nested Case-Control Study [
15] This study found out that two- thirds of the perinatal deaths occurred at first 24hrs of life, therefore, this time represent a critical period in the life of a newborn this was consistent with the study findings on Meta-Analysis of Selected Maternal and Fetal Factors for Perinatal Mortality in Ethiopia [
16].
Partograph was utilized in about half of the mothers who lost their infants; however, utilization of Partograph is likely to reduce labor complications and stillbirths as recommended by the World Health Organization.
The common reported contributors of perinatal mortality were birth asphyxia, prematurity and low birth weight these were in consistency with the findings on perinatal death beyond 41 weeks pregnancy: an evaluation of causes and substandard care factors as identified in perinatal audit in the Netherlands [
17].
According to this study, more perinatal deaths were recorded at level 5 level facility, this is likely to be contributed by the late referrals of critically ill babies from the lower tiers and this facility is the major referral facility in the County.
Study limitations
Despite of the study limitation like some missing information in the abstracted data, the study appears to have a number of strengths; our findings deduced that PNMR in Nakuru was higher than the World Health Organization´s recommendation of below 12 deaths per 1000 live births[
18] and the study could identify contributors of perinatal mortality in Nakuru County that were in agreement with other studies´ findings.
Recommendations
There is a need for Nakuru County: To enhance perinatal mortality surveillance at all facility levels, identify strategies to reduce incidences of asphyxia, prematurity and low birth weight babies, strengthen Health care workers on records and data quality to ensure valid inferences drawn from them and to sensitize and capacity build Health staffs on Partograph use and to increase resource allocation towards maternal child health.
Conclusion


Nakuru County PNMR was higher compared to WHO recommendation of below 12 deaths per 1000 live births[18] and the common causes of perinatal deaths were birth asphyxia, prematurity and low birth weight.
Perinatal mortality rate serves as the most sensitive index of maternal and neonatal care. Therefore: Consistent utilization of Partograph, comprehensive antenatal coverage and adequate care with optimal management of infants at birth are likely to reduce PNMR and improve quality of life among the survivors.
What is known about this topic
- The PNMR is five times higher in developing than in developed nations (10 per 1000 and 50 per 1000 total births in developed and developing countries respectively).
- Studies have demonstrated that, in developing countries; obstructed labor, birth asphyxia, abnormal fetal presentation, underweight and pre enclampsia in pregnancy are known to increase the risk of perinatal mortality by more than five times and all these may account for more than one-third of all perinatal deaths.
- Perinatal mortality rate (PNMR) is considered as one of the indicators of the health status of a given society and it depends on the quality of health care provided to the pregnant women and their babies.
What this study adds
- It will give an insight on the possible contributors to perinatal deaths in Nakuru County and its findings will inform policy to identify strategies and interventions aimed at enhancing survival of neonates, improve quality of care and accessibility of new-born care services hence curbing perinatal morbidity and mortality in the county.
- This study will inform Nakuru County Health Management Team (CHMT) to know where gaps exists in the perinatal surveillance in health care facilities hence they will in turn put their attention towards strengthening perinatal surveillance in the county like sensitizing health workers on complete data entry, timely reporting and data quality audit.
- It will alert Nakuru country health policy makers to study and act on factors behind low Partograph use.
Competing interest


The authors declare no competing interests.
Authors' Contribution


BN participated in the conceptualization of the study, YR helped in data abstraction from KHIS, and we were supervised by ZG. All the authors participated in data entry and analysis. BN drafted the manuscript. All authors reviewed the manuscript, have read and approved the final manuscript.
Acknowledgement


We thank the Nakuru County health teams and the County Epidemiologist officer for availing data to us.
The Field Epidemiology and Laboratory Training Program (FELTP) for providing technical support and we also thank our supervisors for their inputs, critical and constructive reviews during development of this manuscript.
We also thank the Biostatistician from Kenya Medical Research Institute (KEMRI) for the additional information and support he gave us during data analysis.
Tables and Figures


Table 1: Perinatal mortality rate per facility, Nakuru County, Kenya, 2014–2017, N=929
Table 2: Proportion of Partograph use on pregnant women per facility in Nakuru County, 2014–2017
Table 3: Reported contributors of perinatal mortality in Nakuru County, 2014–2017, n=929
Figure 1: Distribution Emergency Obstetric Health care facilities with respective perinatal mortality rate in Nakuru County in Kenya, 2014–2017.
Figure 2: Perinatal mortality rate per year in Nakuru County, 2014–2017
Figure 3: Proportion of perinatal deaths per age, Nakuru County, Kenya, 2014–2017
References


- WHO. Maternal and perinatal health. WHO. 2017. Accessed April 2019.
- Lawn J; Kerber K. Opportunities for Africa's Newborns: Practical Data Policy and Programmatic Support for Newborn Care in Africa. WHO. Accessed May 2019.
- Fink G, Günther I, Hill K. The effect of water and sanitation on child health: evidence from the demographic and health surveys 1986-2007. Int J Epidemiol. 2011 Oct; 40(5):1196-204.https://doi.org/10.1093/ije/dyr102. Google Scholar
- Lehtonen L, Gimeno A, Parra-Llorca A, Vento M. Early neonatal death: A challenge worldwide. Semin Fetal Neonatal Med. 2017; 22(3):153-60. https://doi.org/10.1016/j.siny.2017.02.006. Google Scholar
- Mason E, McDougall L, Lawn JE, Gupta A, Claeson M, Pillay Y, et al. From evidence to action to deliver a healthy start for the next generation. The Lancet. 2014 Aug; 384(9941):455-67.https://doi.org/10.1016/S0140-6736(14)60750-9 Google Scholar
- Shah R, Sharma B, Khanal V, Pandey UK, Vishwokarma A, Malla DK. Factors associated with neonatal deaths in Chitwan district of Nepal. BMC Res Notes. 2015 Dec; 8:818.https://doi.org/10.1186/s13104-015-1807-3. PubMed | Google Scholar
- Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? The Lancet. 2005 Mar; 365(9462):891-900.https://doi.org/10.1016/S0140-6736(05)71048-5. Google Scholar
- Wang H, Bhutta ZA, Coates MM, Coggeshall M, Dandona L, Diallo K, et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016 Oct; 388(10053):1725-74. https://doi.org/10.1016/S0140-6736(16)31575-6. PubMed | Google Scholar
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet Lond Engl. 2010 May 8; 375(9726):1609-23.https://doi.org/10.1016/S0140-6736(10)60518-1. Google Scholar
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet Lond Engl. 2016 Feb; 387(10018):587-603.https://doi.org/10.1016/S0140-6736(15)00837-5. Google Scholar
- Darmstadt GL, Kinney MV, Chopra M, Cousens S, Kak L, Paul VK, et al. Who has been caring for the baby? Lancet Lond Engl. 2014 Jul; 384(9938):174-88. https://doi.org/10.1016/S0140-6736(14)60458-X. Google Scholar
- World Bank. Levels & Trends in Child Mortality Inter-agency Group for Child Mortality Estimation United Nations Levels & Trends in Child Mortalit Report 2014 Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. World Bank. 2016. Accessed Mar 2019.
- WHO, J Åhman E. Neonatal and perinatal mortality: country, regional and global estimates. Geneva: World Health Organization; 2006. 69 p.
- UNICEF, 2015. Maternal and Newborn Health Disparities in Kenya. ReliefWeb. 2015. Accessed Dec 2019.
- Yirgu R, Molla M, Sibley L, Gebremariam A. Perinatal Mortality Magnitude, Determinants and Causes in West Gojam: Population-Based Nested Case-Control Study. PLoS ONE [Internet]. 2016 Jul; 11(7): e0159390.https://doi.org/10.1371/journal.pone.0159390. PubMed | Google Scholar
- Berhan Y, Berhan A. A Meta-Analysis of Selected Maternal and Fetal Factors for Perinatal Mortality. Ethiop J Health Sci. 2014 Sep; 24(0 Suppl):55-68.https://doi.org/10.4314/ejhs.v24i0.6S. PubMed | Google Scholar
- Kortekaas JC, Scheuer AC, de Miranda E, van Dijk AE, Keulen JKJ, Bruinsma A, et al. Perinatal death beyond 41 weeks pregnancy: an evaluation of causes and substandard care factors as identified in perinatal audit in the Netherlands. BMC Pregnancy Childbirth. 2018 Sept; 18:380. https://doi.org/10.1186/s12884-018-1973-0. PubMed | Google Scholar
- WHO. Neonatal mortality. World Health Organization. 2020. Accessed Aug 2020.