Pattern and determinants of self-medication among pregnant women attending antenatal clinics in primary health care facilities in Ogbomoso, Oyo State, Nigeria
Olaniyan Akintunde Babatunde1,2,&, Ikeola Adejoke Adeoye3, Aishat Bukola Usman4, Chukwuma David Umeokonkwo5, Olufunmilayo Ibitola Fawole3
1Oriire Local Government Health Authority, Ikoyi-Ile, Oyo State, Nigeria, 2Nigeria Field Epidemiology and Laboratory Training Programme, Asokoro, Abuja, Nigeria, 3Department of Epidemiology and Medical Statistics, Faculty of Public Health, College of Medicine, University of Ibadan, Oyo State, Nigeria, 4African Field Epidemiology Network, Asokoro, Abuja, Nigeria, 5Department of Community Medicine, Alex Ekwueme Federal University, Teaching Hospital, Abakaliki, Ebonyi State, Nigeria
&Corresponding author
Olaniyan Akintunde Babatunde, Oriire Local Government Health Authority, Ikoyi-Ile, Oyo State, Nigeria. tundebabson23@gmail.com
Introduction:
Self medication in pregnancy has continued to be on the front burner of the global public health discourse due to the increased incidence of abortion, foetal malformation and antimicrobial resistance that were found to be associated with it. Inspite of this burden, in Nigeria, most studies on self-medication were conducted on the general population with only a few carried out among pregnant women. Therefore, this study was carried out to determine the prevalence and factors associated with self-medication among pregnant women in Oyo State.
Methods:
The study was a hospital-based cross-sectional survey. A multi-stage sampling technique was used to select 347 pregnant women who attended antenatal clinics at 56 primary health care facilities in Ogbomoso. A semi-structured, interviewer-administered questionnaire was used to obtain information on the practice of self-medication. Data were analyzed using SPSS version 25; bivariate analysis was done using Chi-square and binary logistic regression was used to identify the predictors of self-medication in pregnancy. The level of statistical significance was set at p < 0.05.
Results:
The mean age of the respondents was 27.0 ± 6 years. The majority (76.6%) of the respondents had poor knowledge of self-medication. About half of the respondents self-medicated with the analgesics (83.1%), antibiotics (66.7%) and antimalarial drugs (28.9%). Nausea and vomiting (90.4%), diarrhoea (67.8%), back pain (62.1%) and fever (28.8%) were the common medical problems. The main reasons for self-medication were previous experience with the drugs (50.9%), the suggestion by family about the drugs (45.2%) and advice from the community pharmacists (31.6%). The proportion of the respondents who used herbal concoction was 30.0% and the reasons given for the herbal use were low cost (47.6%) and perceived efficacy (42.9%). The proportion of pregnant women who gave a history of abnormality in the previously born baby (ies) was 13.0%. Cleft lip (66.7%) was the most prevalent abnormality. The determinants of self-medication were age (aOR: 0.7, 95% CI: 0.33- 0.97), education (aOR: 0.7, 95% CI: 0.49 - 0.99), confidence in other health workers' prescription (aOR: 0.4, 95% CI: 0.15 –0.88), relief from discomfort (aOR: 2.8, 95% CI: 1.46 –5.42) and suggestion by families (aOR: 3.6, 95% CI: 1.62 – 8.05).
Conclusion:
The prevalence of self-medication was high and was more pronounced among married, urban dwellers and those with post-basic education including the respondents aged 25 years and above. This may be explained by the higher proportion of the respondents with poor knowledge of self-medication. Health education, especially during antenatal clinics, on the dangers associated with self-medication in pregnancy, is therefore recommended.
Introduction

The use of orthodox drugs to treat self-diagnosed symptoms, disorders, recurrent or minor health challenges without physician´s prescription is called self-medication [1]. Globally, self-medication is now seen as a public health concern due to the high prevalence of drug misuse and its associated problems such as addiction, adverse drug reactions and masking of disease, which can complicate diagnosis [1,2]. Yearly, the World Health Organization estimated that about 80 to 180 billions of dollars were expended in treating adverse drug reactions caused by self-medication [3]. The manifestation and effects of self-medication are different and may be influenced by the kind of drugs used and even the trimester of the pregnancy [4]. Of great concern is the development of microbial resistance, especially in the developing nations, where antibiotics can be procured over the counter without prescription [5].
The current global economic meltdown has further increased the abuse of drugs and this has led to the increasing practice of self-medication noticed in the general population [
6]. The attendant problems of this rise have become a source of great concern due to the increased incidence of foetal malformation, abortion as well as maternal morbidity and mortality in the communities [
6].
Worldwide, self-medication is a common phenomenon and has been said to be on the increase [
7]. Rahman et al reported that about 80% of the population in the world practiced self-medication, with different proportions across nations; 93% in Slovenia [
8], 87% in India [
9], and 35% in Iran [
10]. In low-income countries, the practice of self-medication also varies and was 46.2% [
11], 69.4% [
12], 59.9% [
13] and 68.9% [
14] among pregnant women in Tanzania, Ethiopia, Democratic Republic of Congo and Ghana respectively. In Nigeria, a prevalence of 62.9% [
15], 67% [
16], 72.4% [
7] and 92.3% [
17] were documented among pregnant women in different parts of the country.
In Nigeria, the practice of self-medication among pregnant women is a major public health concern, as many pregnant women now procure drugs over the counter for self-treatment instead of seeking for health services where medications will be used according to the physician´s prescription. Self-medication is partly accountable for why pregnant women seek medical care late, thereby complicating their conditions and increases the incidence of birth defects. It is estimated that more than 10% of birth defects are caused due to the exposure of pregnant women to drugs [
18].
Many studies have attributed the rising burden of self-medication partly to lack of functional health institutions [
19] and regulatory functions by professional bodies [
20]. In addition, the poor attitude of staff in public healthcare clinics, as well as the cultural beliefs have contributed to self-help using self-medication [
4]. In Nigeria, many studies on self-medication were conducted in the general population [
21-23] while only a few studies conducted on self-medication in pregnancy were mostly carried out in tertiary health facilities [
15,
24,
25].
Tertiary health facilities are largely located in urban centers and accessed mostly by people of high socio-economic status, primary health care facilities, on the other hand, are accessed by both rural and urban dwellers because they are located in both areas and are utilized by the low- and middle-income individuals. Hence, this study assessed the pattern and factors associated with self-medication among pregnant women attending antenatal clinics in primary health care facilities in Ogbomoso, Oyo State.
Methods


Study area: The study was conducted in Ogbomoso, Oyo State. It is situated in the South-western region of Nigeria. It is the second-largest city in Oyo State after Ibadan, the State headquarter. It has five Local Government Areas (LGAs); two urban and three rural. According to Nigeria 2019 projected population, Oyo State has a population of 8,635, 793 while Ogbomoso has a population of 1, 015, 332 using a growth rate of 3.4% and 2006 population figure as the baseline [26]. The estimated population of women of reproductive age group and pregnant women in Ogbomoso was 223, 373 and 50,766 respectively [27]. The inhabitants of the city are majorly Christians and Muslims who mostly engaged in trading, farming and civil service. There are two tertiary hospitals (1 public and 1 private), three general hospitals and one hundred and eight (108) primary health care facilities in Ogbomoso. There are 107 registered patent medicine stores in Ogbomoso. Drug vendors and herbal medicine dealers are common in the rural LGAs.
Study Setting: Ogbomoso comprises of Oriire, Surulere, Ogo-Oluwa, Ogbomoso North and Ogbomoso South LGAs with 31, 28, 23, 14 and 13 health facilities respectively. There are three types of health facilities in the LGAs; primary health care centre, primary health clinic and health post. There are 10 primary health care centres (1 per ward) in each of the LGAs, while each ward has an average of 1 to 3 primary health clinics and health posts. The health facilities were populated by different cadres of the workforce; Primary Health Care Coordinators (these consist of Medical Officers of Health or in their absence, the most senior health workers), Nurses/Midwives, Community Health Officers (CHOs), Community Extension Workers (CHEWs), Medical Laboratory Scientists, Medical Record Officers, Pharmacy Technicians, Health Assistants and Attendants. Activities carried out in these health facilities include; antenatal clinic, infant welfare clinic, immunization services, nutritional services, laboratory services, health education, treatment of common diseases, etc. Antenatal clinics (ANCs) are conducted once a week in all the health centres and managed by the officer-in-charge of the facility who could be a matron or CHO/CHEW. There is a 24-hour daily operation in a few of the health facilities while the majority do not have human capacity for such operation. The coverage rate of the facilities depends on so many factors and those facilities located in the urban areas had higher patronage than their rural counterparts.
Study design: The study was a descriptive cross-sectional survey of primary health care facilities in the local government areas of Ogbomoso, Oyo State.
Study population: The study populations were pregnant women attending antenatal clinics in primary health care facilities in Ogbomoso at the time of the study.
Inclusion criteria: The inclusion criteria were consenting women who attended antenatal clinics in the primary health care facilities within the study period were recruited for the study.
Exclusion criteria: The exclusion criteria were pregnant women who were too ill to provide information, those who were in labour and those with obstetric emergencies.
Sample size calculation: The minimum sample size was calculated using the sample size formula for estimating a single proportion. Based on the proportion of 70.4% from a study conducted on self-medication among pregnant women in Ethiopia [
28], a prevalence of 70.4% was used and margin of error was set at 5%. A non-response rate of 10% was adjusted for; hence, a minimum sample size of 347 was re-calculated.
Sampling technique: A multi-stage sampling technique was used. In stage 1, four LGAs were selected by ballot from five LGAs. In stage 2, a list of all primary health care facilities providing antenatal services in each of the selected four LGAs was made. Half (50.0%) of the health facilities from each of these LGAs were selected making 56 health facilities in all. The number of pregnant women interviewed was proportionately allocated among the health facilities. In stage 3, a systematic random sampling technique was used to select eligible respondents waiting to receive antenatal care from each of the health facilities. The first respondent in each of the health facilities was selected by simple random sampling through a ballot. Subsequently, every 6th respondent was selected until the desired sample size was met. If a selected pregnant woman declined, the respondent with next number replaced her.
Pre-test: The instrument was pretested in two LGAs different from the ones used for the main study. The pretest helped to assess the appropriateness of the questions in eliciting responses from participants. Ambiguous questions were either removed or re-phrased in line with study objectives.
Data collection method and study instrument
Study instrument: Data were collected using a semi-structured, interviewer-administered questionnaire. The questionnaire was developed based on the findings from previous studies in Nigeria [
7,
15,
16]. The questionnaire was administered in English language. It was first translated to Yoruba language and then back-translated to English language to ensure the original meanings of the questions were maintained. The instrument consists of five sections; socio-demographic characteristics, obstetric history, drugs use, medical conditions for which those drugs were used, knowledge of self-medication.
Data collection method: Nine Community Health Extension Workers (CHEWs) and midwives who were Primary Health Care (PHC) staff assisted with data collection. They were trained for 2 hours daily over a 2-day period by the principal investigator on questionnaire administration and research ethics. The training involved pretest on how to maintain privacy during questionnaire administration. A total of 347 study participants were recruited and interviewed between April and May 2019.
Study Variables
(a)
Dependent variable:The primary outcome measure of the study was self-medication and assessed by ‘Yes’ or ‘No’ responses (Yes, the use of any drug without a doctor´s prescription in the current pregnancy).
(b)
Independent Variables:
Socio-demographic characteristics: Age (<25, ≥25 years), marital status (single, married, divorced, separated, widowed), religion (Christianity, Islam, others), tribe (Yoruba, Igbo, Hausa/Fulani, others), educational status (nil formal education, primary, secondary, tertiary), occupation (unemployed, farming/trading, government employee, private employee), monthly income (<18,000, ≥18,000) and place of residence (rural, urban).
Obstetric History: Gestational age (first trimester, second trimester, third trimester), history of pregnancy loss (yes, no) and history of the previous baby with abnormalities (yes, no).
Other variables: Health care costs, advice from others, doctor´s availability in the health facility, access, health facility factors (queues, attitudes and distance), previous experience, transportation cost, knowledge of self-medication, availability of patent medicine stores, advertisement, busy schedule, minor illnesses.
Data analysis: The data were checked daily on the field and Statistical Package for Social Sciences (SPSS) version 25 (SPSS Inc, Chicago, IL, IBM Version) was used for entry and analysis. Data were presented using frequency distribution tables and charts. The association between self-medication and other categorical variables was assessed using Chi-square. In the multivariate analysis, a stepwise model of binary logistic regression analysis was done. Variables imputed into the model were selected if they were significant at the bivariate level. Adjusted odds ratio and 95% confidence interval were reported. Factors that significantly predicted the use of self-medication were reported.
Knowledge Score
Respondents´ knowledge of self-medication was assessed using 4 questions with a total of 15 stem questions. Each correct response was scored one point while each wrong response was scored zero. The total obtainable score was 15, a score above or equal to the mean score (9.0) was categorized as good knowledge. The Cronbach´s alpha coefficient of the knowledge questionnaire was 0.76 in our sample, indicating acceptable internal consistency. This scoring system agrees with a study on knowledge of self-medication in pregnancy among Nigerian residents [
7].
Ethical approval and consent to participate
Approval for the study was obtained from the Ethical Review Committee, Oyo State Ministry of Health (No: AD13/479/1215). All participants were informed about the study and confidentiality protocols. Written Informed consent was obtained from all the participants and the parents of participants under 18 years old.
Results


In all, 347 pregnant women were recruited and interviewed, giving a response rate of 100%.
Socio-demographic characteristics of pregnant women attending antenatal clinics
The mean age of the respondents was 27.0 ± 6 years, 121 (34.9%) were young people, 226 (65.1%) belonged to age 25 years and above. Most were married 304 (87.6%) and more than half 190 (54.8%) were Christians. Little above half 182 (52.4%) had secondary education, while 39 (11.2%) of them had no formal education. More than half (55.3%) of the respondents engaged in farming and trading, while 16.7% were unemployed. Many 144 (41.5%) of the respondents earned below minimum wage (N18, 000) and about two-thirds 228 (65.7%) were urban dwellers. The proportion of government and private employees among the respondents´ husbands was 33 (9.5%) and 64 (18.4%) respectively
Table 1.
Knowledge of self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
The proportion of pregnant women who had poor knowledge of self-medication was 76.6% while 23.4% had good knowledge of self-medication
Figure 1.
Drug history among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
Of the 347 pregnant women interviewed, 177 (51.0%) practised self-medication during the current pregnancy while 105 (30.3%) used herbal concoction together with self-medicated drugs. The most common reasons for the practice of self-medication were the respondents´ previous experience 90 (50.9%) and suggestion by family members 80 (45.2%). These drugs were commonly sourced from the patent medicine stores 144 (81.4%) and leftover of previous prescriptions 17 (9.6%). The use of herbs in combination with the self-medicated drugs was as a result of the associated low cost 50 (47.6%), perceived efficacy 45 (42.9%) and safety 40 (38.1%) of the herbs. The information need on the dosage of drugs for self-medication was given mainly by family members 90 (50.9%) and respondents´ previous experience 70 (39.6%). In the course of self-medication, 79 (44.6%) of the respondents changed their drugs during self-medication. Reasons for the change of drugs were mainly as a result of the exhaustion of former drugs 110 (62.1%), better potency 100 (56.5%) and high cost 98 (55.4%). The majority 226 (76.6%) of the respondents had poor knowledge of self-medication
Table 2.
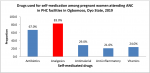
Commonly used drugs for self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
Self-medication was commonly done using analgesics (83.1%), antibiotics (66.7%), antimalarial (28.9%), vitamins (23.7%) and anti-inflammatories (21.7%), vitamins (23.7%) and herbal preparation (11.3%)
Figure 2.
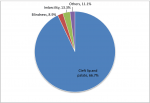
Medical conditions for which self-medicated drugs were used among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
Respondents practiced self-medication to treat medical conditions such as nausea and vomiting (90.4%), diarrhoea (67.8%), back pain (62.1%) and fever (28.8%), respiratory symptoms (15.3%) and Sexually Transmitted Infections (5.6%),
Figure 3.
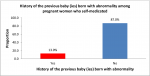
History of the previous baby(ies) born with abnormality(ies) among pregnant women who self-medicated
The proportion of pregnant women who gave a history of previous babies born with abnormalities was 13.0%
Figure 4. Of this proportion, cleft lip and palate (66.7%) and imbecility (13.3%) were the most prevalent conditions
Figure 5.
Determinants of self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
The proportion of respondents that self-medicated was significantly lower among pregnant women aged 25 years and above (70.6%) compared with those less than 25 years (p =0.009). The practice of self-medication was significantly higher among Yorubas (76.8%) compared with other tribes (p < 0.001). The proportion that self-medicated was higher among the respondents with post-basic education (68.4%) as compared with those with primary education and below (p < 0.001). The proportion that self-medicated was significantly higher among those that received more than minimum wage (N18, 000) as monthly income (64.4%) compared with those who received below minimum wage (p < 0.001); it was also significantly higher among the urban dwellers (70.6%) compared to rural dwellers (p < 0.001).
The proportion of respondents that practiced self-medication was significantly lower among the respondents who had patent medicine dealers in the neighbourhood (44.6%) (p < 0.001), treatment cost (33.9%) (p < 0.001), the attitude of health workers (29.9%) (p = 0.002), the suggestion by friends and families about the drugs (35.0%) (p < 0.001) and busy schedule (48.0%) (p < 0.001); but the proportion of self-medication was significantly higher among the respondents who had confidence in other health workers´ prescription (79.9%) (p < 0.001), good knowledge of self-medication (76.5%) (p < 0.001) and those that saw the need to see a doctor for a minor illness (57.6%%),
Table 3&
Table 4.
In multivariate logistic regression analysis, the determinants of self-medication practice among the respondents were age, level of education, opinion of friends and families, confidence in other health workers´ prescription. Younger age (<25 years) were 0.7 times less likely to self-medicate compared with respondents with older age (aOR: 0.7, 95% CI: 0.33- 0.97), respondents with the lower educational background (primary and below) were 0.7 times less likely to self-medicate than those with post-basic education (aOR: 0.7, 95% CI: 0.49 - 0.99) and those who had confidence in other health workers´ (non-physician) prescription were 0.4 times less likely to self-medicate compared with those who had no such confidence (aOR: 0.4, 95% CI: 0.15 - 0.88) while those who wanted to get a quick relief from discomfort were 2.8 times more likely to self-medicate than those who did not want quick relief (aOR: 2.8, 95% CI: 1.46 - 5.42) and those who seek suggestion of friends and families were 3.6 times more likely to self-medicate (aOR: 3.6, 95% CI: 1.62 - 8.05),
Table 3&
Table 4.
Discussion


The study assessed the pattern and determinants of self-medication among pregnant women attending antenatal clinics in primary health facilities in Oyo State, Nigeria. About half of the respondents practiced self-medication and this could be related to the poor knowledge demonstrated, as more than two-thirds of the respondents had poor knowledge of the dangers of self-medication. The poor knowledge reported in our study was consistent with findings from several studies of the same population [23,29], but at variance with 87.6% documented as good knowledge in a Nigerian study [15]. The practice of self-medication was equally informed by the opinion of family members about the medication and the previous experience of the respondents [15,30]. These findings suggest that health education of family members and sensitization on the dangers of self-medication should be given a priority if we must reduce the rising profile of drug resistance, infant and maternal mortalities in our communities.
The prevalence reported in our study was consistent with the findings of studies in Iran (54.4%%) [
31], Yemen (54.1%) [
32] and Nigeria (51.6%) [
23] in the same population but lower than what was documented in some Nigerian studies [
21,
22,
33]. This difference could probably result from different study populations resulting from different socio-economic characteristics. However, the study results were found to be higher than 35.0%, 31.0% and 27.5% reported in Iran, India and Ethiopia respectively [
10,
34,
35]. The higher prevalence in this study could be due to poor knowledge about self-medication and perhaps different study populations.
In this study, commonly self-medicated drugs were majorly sourced from the patent medicine stores and mostly consumed during the first trimester. This is consistent with some findings in Nigerian studies [
16,
36]. In Nigeria, availability of patent medicine dealers and easy access to drugs have been found to increase the practice of self-medication, as the patient often use the prescription for previous ailments to procure drugs for the treatment of their presence illnesses. Information on the dosage of these drugs was majorly given by families and friends, as well as respondents´ previous experience. In the same vein, about half of the respondents arbitrarily changed their drugs in the course of self-treatment and this was majorly due to running out of drugs, perceived efficacy and lower cost. This unsavory practice could lead to the development of antimicrobial resistance when antibiotics are the agents utilized. The finding in this study corroborated one finding that documented wrong dosage and incomplete duration of treatment course as enabling factors for antimicrobial resistance [
37].
In this study, the history of abnormality among the previous baby(ies) born to the pregnant women who self-medicated was 13.0% and this was not surprising due to the higher prevalence of self-medication practice during the first trimester; the period of organogenesis. It is estimated that more than 10% of birth defects are caused due to the exposure of pregnant women to drugs [
18]. However, further studies needed to establish whether the cause of abnormality in the previous baby(ies) born to the pregnant women who self-medicated was only due to previous drug exposure in early pregnancy.
The medical conditions for which drugs were consumed were consistent with some studies in developing countries [
7,
25]. These findings were not surprised because pregnancy is usually accompanied by nausea, vomiting, back and waist pain; pregnant women often self-medicate to treat these ailments as well. This also agreed with another Nigerian [
7] and Ethiopian [
38] studies where fever, pain, infection, stomach upset and bowel irregularity were reported as medical conditions for self-medication.
The determinants of self-medication were age, educational level, confidence in other health workers´ prescription, quick relief from discomfort and opinion of friends and families. Those aged less than 25 years were one-third less likely to practice self-medication, compared with those aged 25 years and above [
16]. In the Southwestern part of Nigeria, there is a delay in women marriage because of educational career, hence, majority of them became pregnant for the first time at an older age and do not know pregnancy-related symptoms. As a result of their naivety, they often self-medicate to treat these symptoms. It is essential for the health workers in charge of antenatal clinics in primary health care facilities to reiterate more on the symptoms associated with early pregnancy and the need to seek medical advice from the professionals rather than embarking on self-treatment. This will go a long way in reducing pregnancy-related complications, especially in the first trimester.
Low educational background is most times synonymous with poverty and unemployment and the respondents belong to this category were one-third less likely to practice self-medication, compared with those with post-basic education [
16]. No wonder the high prevalence (30.3%) of herbal medicines among the respondents was reported in this study, as many of them attributed its use to financial and safety reasons. This is evidenced as the majority of the respondents could not afford the cost of treatment and transportation to the facilities because nearly half of the respondents lived below the minimum wage of N18, 000 monthly (< 50 US dollar). In view of this, efforts must be geared towards improving the living standard of the populace, especially the pregnant women so as to avoid the fatal complications of self-medication and the use of herbs on the developing foetus.
In addition, respondents practiced self-medication as a result of a lack of confidence in other health workers´ prescription. This was attributed to their claim that doctors were not always available in the health facilities, hence their recourse to self-medication practice. The respondents who had confidence in other health workers´ prescription were about two-thirds less likely to engage in self-medication practices, compared with those who did not have such confidence. Quick relief from discomfort and suggestion by friends and families were also found to be determinants of self-medication practices among the respondents; with respondents that preferred quick relief from discomfort were about 4 times more likely to practice self-medication, compared with those who did not; and respondents with a suggestion by friends and families were about 3 times more likely to practice self-medication, compared with those with no such suggestion. These factors have also been identified as determinants of self-medication practices in several studies conducted in Nigeria and other places [
7,
25,
34,
39].
These findings highlight the importance of physicians in our health facilities as it enables the respondents to overcome the barriers of confidence in the areas of drug´s prescription due to non-availability of doctors in health facilities. Establishment of non-availability of doctors among the respondents in this study exposes the gross inadequacies in the allocation of human resources for the provision of effective and efficient healthcare services in Nigeria. This finding emphasizes the need for government to make enough resources available to the health sector to enable it to provide comprehensive healthcare services to the populace, particularly pregnant women.
The communal belief that herbal medicine has better safety and efficacy than orthodox medications as well as the high positive history of previous babies with abnormality calls for serious concern in these studies. Regulation of herbal medicine and proper education of dangers of self-medication on the mothers and the unborn babies must be given adequate priority if we must have a productive and healthy society. Several studies conducted among different populations across Nigeria also reported financial constraints as one of the most common reasons for self-medication [
36,
40,
41]. It is therefore imperative that the government should scale-up service delivery, especially in the area of health education in the antenatal clinics.
Limitations of the study
The information given by respondents limited our study since it was a questionnaire-based survey. Secondly, it was difficult for some subjects to mention the names of the drugs which they used for self-medication. To reduce this problem, efforts were put in place to use the colour and size of the drugs for identification during the interviews. Thirdly, the study excluded other public health facilities (secondary and tertiary), private health facilities and pregnant women who were not attending antenatal clinic since the research was hospital-based. The perceived effect of this was reduced through health education and sensitization of the gatekeepers and other community leaders on the need to ensure that women come for antenatal services at the primary health care facilities.
Conclusion


Prevalence of self-medication among pregnant women attending antenatal clinic in Ogbomoso was high and was more pronounced among married, urban dwellers and those with post-basic education including the respondents aged 25 years and above. This may be explained by the inadequate knowledge of self-medication shown among the respondents. Health education on the dangers of self-medication in pregnancy is recommended in all the antenatal clinics of primary health care facilities in the state.
What is known about this topic
- Self-medication is now considered as one of the public health issues because of medical and socio-economic implications such as abortion, drug resistance, fetal malformation, adverse drug reactions and addiction.
- Lack of adequate knowledge is also known to contribute to the increased prevalence of self-medication among pregnant women in Nigeria.
- The factors responsible for self-medication in the general population and among pregnant women attending antenatal clinics in tertiary and secondary health facilities, but not much among the attendees of antenatal clinics of primary health centres with a different socio-economic background.
What this study adds
- Aside self-medication with orthodox medicine, this study was able to record a high prevalence of herbal use which negatives some findings documented in secondary and tertiary health facilities.
- The study adds that age less than 25 years, primary school education and below, confidence in other health workers' prescription were factors associated with the low practice of self-medication while quick relief from discomfort and suggestion by friends and families were associated with the high practice of self-medication in pregnancy.
- Prevalence of self-medication in pregnancy used to be lower compared with the general population but this study equally documented high prevalence of self-medication among pregnant women in these areas.
- From the literature, some of the factors that increase the odds of self-medication practice among pregnant women attending antenatal clinics in tertiary health facilities were seen as protective variables in our study.
- Holistic health education of pregnant women during antenatal clinics on the danger associated with self-medication and the use of herbs.
Competing interests


The authors declared no competing interests.
Authors' contributions


OAB conceptualized the study, OIF and IAA contributed to the design. OAB drafted the initial manuscript, OAB, OIF, IAA, ABU and CDU contributed to the analysis and interpretation of the results and made a substantial revision to the initial draft. All authors read and approved the final version of the manuscript.
Acknowledgements


The authors appreciate the Head of Local Government Administration, PHC Technical Committees, Officers-in-charge of health facilities where the study was conducted and the pregnant women that participated in the study for their cooperation.
Tables and figures


Table 1: Socio-demographic characteristics of pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019 (N = 347)
Table 2: Drug history of pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo state, 2019 (N =347)
Table 3: Determinants of self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019 (N =177)
Table 4: Determinants of self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State (N =177)
Figure 1: Knowledge of self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
Figure 2: Drugs used for self-medication among pregnant women attending ANC in PHC facilities in Ogbomoso, Oyo State, 2019
Figure 3: Medical conditions among pregnant women attending antenatal clinic in PHC facilities in Ogbomoso, Oyo State, 2019
Figure 4: History of the previous baby (ies) born with abnormality(ies) among pregnant women who self-medicated
Figure 5: Types of abnormalities found among previous baby(ies) born to pregnant women who self-medicated
References


- Dayani G, Luciana MG, Graziela MA, Silvana CT. Responsible self-medication: Review of the process of pharmaceutical attendance. Brazilian J Pharm Sci. 2009; 45(4):625-633. Google Scholar
- Refuerzo JS, Blackwell, Sokol RJ. Use of over-the counter medications and herbal remedies in pregnancy. Am J Perinatol. 2005; 22(6):321-4. Google Scholar
- World Health Organization (WHO). Promoting rational use of medicines: core components. WHO. September 2002. September 2019.
- Fakeye TO, Adisa R, Musa IE. Attitude and Use of Herbal Medicines Among Pregnant women in Nigeria. BMC Complementary and Alternative Medicine. 2009; 9:53-59. https://doi.org/10.1186/1472-6882-9-53. PubMed | Google Scholar
- Chalker J. Improving antibiotic prescribing in Hai Phong Province, Vietnam: the “antibiotic-dose” indicator. World Health Organization Bulletin. 2001; 79(4):313-320. Google Scholar
- GNA. Health News: Health system under serious abuse in Wa Municipality. GNA. May 2010. Accessed October 2019.
- Abasiubong F, Bassey EA, Udobang JA, Akinbami OS, Udoh SB, Alphonsus Udo Idung. Self-Medication: potential risks and hazards among pregnant women in Uyo, Nigeria. Pan African Medical Journal. 2012; 8688:1-8. https://doi.org/10.11604/pamj.2012.13.15.1454 PubMed | Google Scholar
- Klemen-ketis Z, Hladlink Z, kersnick J. Self-medication among health care and non health care students at University of Ljubljana, Slovenia. Department of family medicine. 2010; 19(5):395-401;https://doi.org/10.1159/000316380 . Google Scholar
- Rohit KV, Lahit M, Manisha P. Evaluation of self medication among professional students in northern india:Proper statutory drug control must be implemented. Asian Journal of pharmaceutical and clinical research. 2010; 3(1):60-63. Google Scholar
- Baghianimoghadam MH, Mojahed S, Baghianimoghadam M, Yousefi N, Zolghadr R. Attitude and practice of pregnant women regarding self-medication in Yazd, Iran. Archives of Iranian Medicine. 2013; 16(10):580-583. PubMed | Google Scholar
- Marwa KJ, Njalika A, Ruganuza D, Katabalo D, Kamugisha E. Self-medication among pregnant women attending antenatal clinic at Makongoro health centre in Mwanza, Tanzania: a challenge to health systems. 2018; 18(1):16. https://doi.org/10.1186/s12884-017-1642-8 . PubMed | Google Scholar
- Jambo AM, Getnet S, Mekonnen A, Firehiwot R, Michael JC, Michael L. Self-Medication and Contributing Factors Among Pregnant Women Attending Antenatal Care at Public Hospitals of Harar Town , Ethiopia. Front Pharmacol. 2018; 9:1063. https://doi.org/10.3389/fphar.2018.01063 . PubMed | Google Scholar
- Mbarambara M, Songa B, Wansubi M, Mututa M, Minga BK, Bisangamo K. Self-medication practice among pregnant women attending antenatal care at health centers in Bukavu , Eastern DR Congo. International J of Innovation and Applied Studies. 2016; 16(1):38-45. Google Scholar
- Agyei-Boateng R. Self Medication practices among pregnant women in Ejisu-Juaben Municipality. Kwame Nkrumah University of Science and Technology. 2015. Google Scholar
- Joseph BN, Ezie IJ, Aya BM, Dapar MLP. Self-medication among Pregnant Women Attending Ante-natal Clinics in Jos-North, Nigeria. International Journal of tropical disease and Health. 2017; 21(1):1-7. Google Scholar
- Attahiru Aisha, Awosan K. Joseph, Hassan Mairo, Arisegi S. Adeniyi. Awareness, Risk Perception and Practice of Self-Medication Among Pregnant Women Attending Ante-Natal Clinics in Sokoto, Nigeria. Journal of Drug Delivery and Therapeutics. 2018; 8(4):256-62. https://doi.org/10.22270/jddt.v8i4.1782 . Google Scholar
- Ayanwale MB, Okafor IP, Odukoya OO. Self-medication among rural residents in Lagos, Nigeria. J Med Trop 2017; 19(1):65-71.lhttps://doi.org/10.4103/jomt.jomt_51_16 . Google Scholar
- Nakamura MU, Kulay Junior L, Pasquale M. Uso de fármacos na gravidez: benefício e custo. Rev bras ginecol obstet. 2008; 30(1):1-4.https://doi.org/10.1590/s0100-72032008000100001 . PubMed | Google Scholar
- Baiyewu O. Traditional Medicine and health care Delivery. Nigerian Journal of Psychiatry. 2001; 1(5):284-288.
- Van der Geest S, Hardon A. Self-medication in developing countries. Journal of Social and Administrative Pharmacy.1990; 7(4):199-204.
- Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Annals of African Medicine. 2008; 7(3):120-7.https://doi.org/10.4103/1596-3519.55666 . Google Scholar
- Oluyemi JA, Yinusa MA, Abdullateef R, Sunday A, Kehinde K. Factors influencing the practice of self-medication among bankers in selected new generation banks in Ilorin Nigeria. International Journal of Economics & Management Sciences. 2015; 4(2):1-7.https://doi.org/10.4172/2162-6359.1000227 . Google Scholar
- Auta A, Shalkur D, Omale S, Abiodun AH. Medicine Knowledge and Self-Medication Practice Among Students. African Journal of Pharmaceutical Research & Development. 2012; 4(1):6-11. Google Scholar
- Bello FA, Morhason-Bello IO, Olayemi O, Adekunle AO. Patterns and predictors of self-medication amongst antenatal clients in Ibadan, Nigeria. Niger Med J. 2011; 52(3):153-7. https://doi.org/10.4103/0300-1652.861. PubMed | Google Scholar
- Yusuff KB, Louis-Domeih Omarusehe. Determinants of self medication practices among pregnant women in Ibadan, Nigeria. Int J Clin Pharm. 2011; 33:868-75. https://doi.org/10.1007/s11096-011-9556-4. PubMed | Google Scholar
- Federal Republic of Nigeria Official Gazette. Legal Notice on Publication of 2006 Census Final Results. The Federal Government Printer, Abuja, Nigeria. 2009; 96(2):B1-42.
- Federal Republic of Nigeria. 2019 Nigeria Projected Population by Local Government Areas (based on 2006 National Provisional Results with the State-specific Growthrate). Federal Republic of Nigeria. 2006. Accessed October 2019.
- Endalkachew Worku Mengesha. Drug use and its associated factors among pregnant women in Bahir Dar city administration, Northwest Ethiopia. Sexual and Reproductive Health Care. 2019; 2(1):21-6. Google Scholar
- Sawalha A. Assessment of Self-medication Practice among University students in Palestine: Therapeutic and Toxicity complications. The Islamic University Journal. 2007; 15(2):67-82. Google Scholar
- Tenaw Andualem, Tsige Gebre-Mariam. Self Medication practices in Addis Ababa, A Prospective study. Ethiopian Journal of Health Science. 2004; 14:1. Google Scholar
- Tajik R, Shamsi M, Mohammad Beygee A. Survey prevalence of self medication and factors effected in pregnant woman´s Arak City. Sci J Hamadan Nurs Midwifery Fac. 2008; 16(1):29-39. Google Scholar
- Alkadasia MN, Putaiahb ET. Study of self-medication among pregnant women and associations with socio-demographic data in Al-qaedah district, Ibb, Yemen. J Med Res Health Sci. 2019; 2(3):576-586. https://doi.org/10.15520/jmrhs.v2i3.37 . Google Scholar
- Onajole AT, Bamgbala AO. Socio demographic characteristics of drug misuse in a Polytechnic in Lagos, Nigeria. Nig Jnl Health and Biomed Sciences. 2004; 3(1):40-43. https://doi.org/10.4314/njhbs.v3i1.11506. Google Scholar
- Jain S, Malvi R, Purviya JK. Concept of Self-medication; a Review. International Journal of Pharmaceutical and Biological Archives. 2011; 2(3):831-836.
- Abula T and Worku A. Self medication in three towns of North West Ethiopia. Ethiopian Journal of Health Development. 2001; 15(1):25-30. Google Scholar
- Omolase CO, Adeleke OE, Afolabi AO, Afolabi OT. Self-medication among General Outpatient in Nigerian community hospital. Annual journal of postgraduate medicine. 2007; 5(2):64-6.https://doi.org/10.4314/aipm.v5i2.64032 . PubMed | Google Scholar
- Bennadi D. Self-medication: A current challenge. J. Basic Clin Pharm. 2013; 5:19-23.https://doi.org/10.4103/0976-0105.128253. PubMed | Google Scholar
- Eticha T, Mesfin K, Unnikrishnan B, Rekha T, Mithra P. Self-Medication Practices in Mekelle, Ethiopia. PLoS ONE. 2014; 9(5): e97464. https://doi.org/10.1371/journal.pone.0097464 . PubMed | Google Scholar
- Aswapokee N, Vaithayapichet S, Heller RF. Pattern of antibiotic use in medical wards of a university hospital, Bangkok, Thailand. Rev Infect Dis. 1990; 12(1):136-41. https://doi.org/10.1093/clinids/12.1.136. PubMed | Google Scholar
- Auta A, Omale S, Folorunsho TJ, David S, Banwat SB. Medicine vendors: self-medication practices and medicine knowledge. North Am J Med Sci 2012; 4(1):24-28. https://doi.org/10.4103/1947-2714.92899. PubMed | Google Scholar
- Akinlade KA, Akinyemi JO, Fawole OI. Knowledge of hazards of antibiotic self-medication by mothers for under-fives in rural community of Southwest Nigeria. Afr J Med Med Sci. 2015; 44(4):303-9. PubMed | Google Scholar