Investigation of a cluster of SARS-COV-2 infections among workers in a factory making personal protective equipment, Buikwe District, Uganda, 2020
Aggrey Byaruhanga1,&, Elizabeth Katana1,, Alex Ndyabakira1, Sandra Nabatanzi1, Richard Migisha1, Geoffrey Amanya1, Lilian Bulage1, Daniel Kadobera1, Alex Riolexus Ario1,2, Julie Harris3
1Uganda Public Health Fellowship Program, Ministry of Health, Kampala, Uganda, 2Uganda National Institute of Public Health, Kampala, Uganda, 3US Centers for Disease Control and Prevention, Kampala, Uganda
&Corresponding author
Aggrey Byaruhanga, Uganda Public Health Fellowship, Ministry of Health Uganda, Kampala, Uganda. abyaruhanga@musph.ac.ug
Introduction:
In September 2020, a cluster of SARS-COV-2 infections was reported among workers at a factory making personal protective equipment (Factory X) in Buikwe District, Uganda. The factory had already instituted risk reduction measures, including mandatory wearing of masks and hand sanitizing at all entry points. We investigated the cluster to establish the magnitude and determine exposures associated with transmission.
Methods:
We defined a confirmed case as a positive real time polymerase chain reaction (RT-PCR) test for SARS-COV-2 infection in a Factory X worker during August-September 2020. We identified case-patients through records at the health facility at Factory X. We selected controls randomly from Factory X departments with cases. We conducted a case-control study using a semi-structured, standardized questionnaire and a randomly-selected subset of case-patients from the line list. We used logistic regression to identify the factors associated with SARS-COV-2 infection and obtained adjusted odds ratios (aOR). We conducted informal qualitative interviews with facility staff to understand compliance to prevention measures and used an environmental assessment checklist to identify factory-specific risk factors for infection.
Results:
We established the index case-patient as a 27-year-old employee in the new garments department who became ill on 7 August and whose infection was confirmed on 10 August. We identified 163 cases from 1,500 persons tested 18 August-14 September, 2020 (positivity rate=10.9%); none died. The engineering department was the most affected (positivity rate= 29.8%). Among 75 cases and 75 controls, lack of mask use (aOR= 5.9, 95% CI 2.3-15.8) and working in the old garments (aOR=2.4, 95% CI 1.1-5.5) or engineering departments (aOR=13.5, 95% CI 2.4-75.6) were associated with infection. We observed engineers frequently transiting between all departments at the factory to provide technical services. Among 12 buildings at Factory X, only the administration had adequate windows and doors for ventilation; engineering and old garments departments had no windows.
Conclusion:
This cluster of SARS-COV-2 infections was associated with failure to use masks and working in poorly-ventilated and/or congested areas. The development of Standard Operating Procedures to ensure adherence to face mask use, increased spacing between persons on production lines, improved ventilation, and provision of adequate windows and doors by factory management may help avert future outbreaks.
Introduction

Coronavirus Disease 2019 (COVID-19) disease has frequently been characterized in clusters, largely due to its tendency to spread widely from small numbers of infected persons[1, 2]. Crowded, poorly ventilated settings have provided ample opportunities for Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to spread in workplaces, nightclubs, and churches, among others[3, 4]. Outbreaks and clusters of COVID-19 have also been reported in a variety of occupational settings since the start of the pandemic in Europe and Asia[5, 6] . Large numbers of clusters were reported particularly from processing sectors, in factories and manufacturing and in office settings[7, 8]. This is because, workers in many essential sectors could not work from home, thus standing a high chance of acquiring COVID-19.
On 21 March 2020, Uganda confirmed its first case of COVID-19 in an incoming symptomatic traveler detected during mandatory airport screening [
9]. By 25 November 2020, the country had registered 19,115 cases, 93% of which represented community transmission, from 130 of its 135 districts [
10]. The widespread community transmission was characterized by multiple clusters in factories, health facilities, prisons, and both formal and informal workplaces [
11].
On 26 September 2020, the Ministry of Health (MoH) received information about a cluster of COVID-19 cases among workers at a peri-urban factory responsible for making personal protective equipment in Buikwe, Uganda. In August and September 2020, the district reported a small number of COVID-19 clusters among food vendors along a nearby highway (unpublished data).
We investigated the cluster to establish the magnitude of and exposures associated with transmission of SARS-COV-2 infection among factory workers.
Methods


Outbreak area
Buikwe District is located in central Uganda and has a population of approximately 430,000 persons according to Uganda Bureau of Statistics, 2015 [
12]. As of 15 August 2020, there were 49 confirmed COVID-19 cases in the district and a positivity rate among person tested of 2.7% [
13].
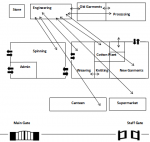
Factory X is located in Buikwe District. It employs 3,000 workers and manufactures personal protective equipment, including face masks, face shields, and coveralls. It is composed of 12 independent departments, including old garments, new garments, engineering, spinning, cotton-weaving, knitting, processing, administration, welfare, canteen, and clinic. The factory has biometric logins (fingerprint-based) for workers in old garments, new garments, and administration. Starting in March 2020, after the first cases of COVID-19 were detected in Uganda, Factory X instituted mandatory wearing of face masks and use of hand sanitizer at all factory entry points to reduce risk of COVID-19 transmission.
The index case-patient
The index case-patient was a 27-year-old man working in the new garments department at the factory who tested positive on 10 August 2020. His positive test prompted the factory to implement random testing of 1,500 factory workers from 18 August to 14 September 2020.
COVID-19 testing
The district laboratory personnel randomly collected samples for COVID-19 testing ten times during 18 August to 14 September, 2020, ultimately covering half of the workers at the factory (1,500 persons). Only half of workers were tested due to shortages of testing kits in the country at the time.
Case definition
We defined a confirmed case as a positive real time polymerase chain reaction (RT-PCR) test for SARS-COV-2 infection in a Factory X worker during August-September 2020. To identify cases, we reviewed medical records from the health facility at the factory and line-listed all persons who met the case definition. These represented persons who were tested randomly by the factory, not persons who sought care because they were symptomatic. We selected the 75 case-patients who were present at the factory during the outbreak investigation for interviews. We described case-patients by person, place, and time. We calculated attack rates (AR) overall, by sex, and by Factory X department.
Observations
During the outbreak investigation, we observed the layout of the factory to establish potential risk factors for SARS-CoV-2 infection. These included adequate work spacing (factory workers seated ?2 meters apart at workspaces), ventilation of the working rooms and cafeteria, and use of biometric entry and exit points for workers. We randomly selected twelve factory workers and held informal discussions with them to understand worker flow and time spent in each department in the factory. We also asked them about their movements within the factory, where they met for daily meal and the availability of COVID-19 SOPs.
Hypothesis generation
Using a semi-structured questionnaire, we interviewed a convenience sample of 20 COVID-19 case-patients at the factory to establish their potential exposures two weeks prior to COVID-19 testing. The exposures of interest included visiting market places, attending places of worship, visiting burial places, means of transport to their respective residences, visiting bars outside of work, wearing masks properly and consistently at work, factory department of work, and working in congested areas.
Case-control study
We conducted a 1:1 unmatched case-control study to test the generated hypotheses using a standardized interviewer-administered questionnaire. We defined a control as a Factory X worker who tested negative for COVID-19 from 15 August-14 September 2020.
Sample size determination
The sample size was calculated based on Kelsey et al [
14]. Using a two-sided significance level of 0.05, a power of 80%, and an estimated 40% of cases and 64% of controls using masks [
15], a sample size of 150 was obtained (75 cases and 75 controls). We selected cases for inclusion using simple random sampling from our line list; controls were selected for inclusion using random sampling from a list of persons who tested negative for COVID-19 at the factory in the departments that had cases.
Data collection procedure
Using a semi-structured questionnaire, we collected data on the exposures indicated as high-risk during hypothesis generation, including the department of work at the factory, transiting to other factory departments during the workday, visits to markets, burials, drinking places during the two weeks before COVID-19 testing, consistent and proper use of masks, and maintaining social distance (at least 2 metres at all times at work). We additionally collected data on the age and sex of the respondents.
Data analysis
We entered the data in EpiInfo version 7.2 and analysed using Stata version 15 software. Descriptive statistics were presented as frequencies and proportions for categorical variables. We used logistic regression to identify risky exposures. Variables that were significant at bivariable analysis were checked for collinearity and included in the multivariable model to estimate independent effects. The model was built using a backward stepwise method. Variables in the final model were considered statistically significant at a p-value <0.05
Availability of data and materials
The datasets used and analyzed during this study belong to the Uganda Public Health Program and are not publicly available. However, the datasets could be made available by the corresponding author upon reasonable request and with permission from the Uganda Public Health Fellowship Program
Ethics approval and consent to participate
A non-research determination was obtained from the US Centers for Disease Control and Prevention to conduct this outbreak investigation. The Ministry of Health (MoH) gave the directive to conduct outbreak investigations for SARS-CoV-2 infection. We sought verbal consent from respondents in their respective languages during data collection. Participants were told that their participation was voluntary and that there would be no negative consequences if they refused to participate (none declined). During data collection, respondents were assigned unique identifiers instead of names to protect their confidentiality. Information was stored in password protected computers and was not shared with anyone outside the investigation team. As this was a public health emergency, disclosure of patient information for the purposes of contact tracing was limited to the minimum needed to conduct contact tracing activities.
Results


Descriptive epidemiology
Of the 1,500 persons tested, 163 tested positive (positivity rate=10.9 %). Between 29 and 394 persons were tested at each visit, with positivity rates among persons tested ranging from 4.5% on August 17 to 17% on September 3
Figure 1.
Of the 163 cases, 39 (24%) were symptomatic with headache, fever, dry cough, chest pain, and/or sore throat; the rest were asymptomatic. None of the case-patients died. The mean age of the case-patients was 27 years (range: 18-60 years). Case-patients came from different departments of the factory, with most coming from old garments (84), new garments (63), and engineering (14). The engineering department (positivity rate: 29.8%) was most affected
Table 1.
Observational findings
During our individual interviews, workers shared that some employees - primarily but not exclusively engineers - moved through many departments in a day, providing technical services across the factory. Most workers met for their daily meals at the canteen and the supermarket. Posters on COVID-19 preventive measures, including face mask use, were present throughout the factory. However, we observed little use of face masks among employees. In addition, we observed many engineering department workers transiting through the factory without wearing face masks
Figure 2. We also noted many people entering the facility at once, leading to frequent crowding around the biometric fingerprint machines. The biometric login machine was not sterilized between users and was at that time considered a possible mechanism of transmitting infection. The biometric login machine was not sterilized between users and was at that time considered a possible mechanism of transmitting infection. We also observed that there was line production in the new and old garment departments, in which each line had at least 10 persons working. These departments had poorly aerated rooms with workers seated <2 meters from the next person. All other departments had adequate ventilation.
Factors associated with SARS-CoV-2 infection
In multivariate analysis, working in the old garments department (aOR=2.4, 95% CI, 1.1-5.5) and the engineering department (aOR=14, 95% CI, 2.4-76) were associated with higher odds of infection, compared to the new garments department
Table 2. Factory workers who self-reported not wearing masks properly and consistently had higher odds of infection (aOR=5.9, 95% CI, 2.3-16) than those who self-reported wearing masks consistently and properly
Table 2.
Discussion


This cluster of infected persons with SARS-COV-2 infection was the largest workplace cluster identified in Uganda since the pandemic began. The identification of a single symptomatic case prompted mass testing, which suggested that approximately 10% of the factory workers were infected. The outbreak was exacerbated by poor adherence to the use of face masks and working in congested, poorly-ventilated environments.
Our investigation revealed that 24% of the infected factory workers were symptomatic with headache, fever, dry cough, chest pain and/or sore throat at the time of testing, suggesting that many people came to work ill despite guidelines to stay home. This is likely related to social stigma in Uganda around testing positive for COVID-19 [
16,
17], as well as possible concerns about the economic impact of missing work [
18]. These issues complicate the ability to prevent workplace infections when workplaces are reliant on self-reporting of symptoms.
Infection rates were highest in the engineering, new garments and old garments departments. The association of infection risk with engineering is likely due to the nature of the engineers´ work, characterized by frequent movement to other departments to provide technical services on the various machines. These movements likely exposed engineers, compared with other cadres of workers, to larger numbers of co-workers. New garments and old garments departments were congested with inadequate ventilation, while other departments were less crowded and had improved ventilation.
Face mask use is well-supported as an intervention to reduce the risk of COVID-19 transmission, especially in congested settings [
19-21]. However, during our seven-day visit, we noted that few workers were wearing masks properly. Similar to previous studies, our analyses confirmed an association between lack of face mask use and acquisition of SARS-CoV-2 infection. Adherence to this guideline is especially important in congested indoor settings without adequate ventilation, and efforts should be made to enforce mask use to reduce workplace infection risk.
The close physical proximity of workers to each other likely also amplified the outbreak. Physical proximity has been well-established as a risk factor for SARS-COV-2 infection previously, and is the rationale for recommending social distancing [
21]. However, factories might find it difficult to implement social distancing measures when it interferes with their production lines. Workplaces with inherently crowded conditions might consider reducing the density of workers with shift work or by staggering working hours to reduce congregation of employees. This might require a tradeoff with efficiency of production, and such workplaces might consider ‘triggers’ for when to implement these measures during periods with higher COVID-19 infection rates.
To reduce COVID-19 workplace outbreaks, workplaces need to address both the risk of introduction and the risk of spread within a factory. It is possible that the index case-patient was the only source of infections at the factory; the epidemic curve indicated an increase in positivity after the index case´s detection. However, it is also possible that there were multiple introductions of COVID-19 into the factory. At the time of this study, the district in which the factory was located had reported approximately 50 SARS-CoV-2 infections. Integration of tracking mechanisms for local infections at workplaces and enhanced focus on preventive measures, including periodic worker monitoring to ensure adherence to preventive measures, may be warranted during higher-risk times to prevent such outbreaks in the future. A primary limitation of our study is that only half the workers in Factory X were tested. It is unknown if the infection rates in these workers represented the infection rates in the entire factory population.
Conclusion


A cluster of SARS-CoV-2 infections among factory workers was likely propagated by non-adherence to face mask use and working in congested areas with poor ventilation. Spread might have been facilitated by persons who came to work while ill. Enforcement of adherence to standard operating procedures such as face mask use, provision of adequate space between production lines, and adequate ventilation by the factory management could reduce the risk of future outbreaks.
What is known about this topic
- Clusters of SARS-COV-2 infections were frequently observed
- Crowded, poorly ventilated settings provided ample opportunities for SARS-COV-2 to spread
- Outbreaks and clusters of this infection were previously reported in a variety of occupational settings such as processing sectors, in factories and manufacturing and in office settings
What this study adds
- This study investigated a cluster of SARS-COV-2 infection among factory workers to establish the magnitude of and exposures associated with the transmission
- This cluster of infected persons with COVID-19 was the largest workplace cluster identified in Uganda
- The outbreak was exacerbated by poor adherence to the use of face masks and working in congested, poorly-ventilated environments
Competing interests


The authors declare no competing interests.
Funding and disclaimer
This project was supported by the President´s Emergency Plan for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention Cooperative Agreement number GH001353-01 through the Makerere University School of Public Health to the Uganda Public Health Fellowship Program, Ministry of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the US Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry (CDC/ATSDR), US Department of Health and Human Services, Makerere University School of Public Health, or the Uganda Ministry of Health.
Authors' contributions


AB, EK, AN, SN, RM, GA, LB, DK, AAR, and JRH contributed to the study design and drafting of the manuscript, AB and EK conducted the data analyses. EK and DK contributed to data collection, and RM, GA, SN, LB, AAR, and JRH contributed to the interpretation of the findings and review of the manuscript. All authors contributed to the write up, and read and approved the final manuscript.
Acknowledgments


We would like to thank the Uganda Ministry of Health for giving us the opportunity to access the COVID-19 database, the CDC for supporting the Uganda Public Health Fellowship Program activities and the factory management for support during the investigation and response.
Tables and figures


Table 1: SARS-CoV-2 positivity rates by sex, department, and overall, at a peri-urban Factory X, Buikwe District, August to September, 2020
Table 2: Exposures for SARS-COV-2 infection among factory workers in a peri-urban Factory X in Buikwe District, August- September, 2020
Figure 1: Distribution of COVID-19 cases by week of sample collection, 8 August to 14 September 2020 in peri-urban Factory X, Buikwe District, Uganda
Figure 2: Diagram illustrating the design of the peri-urban Factory X in Buikwe district, Uganda, with arrows representing the movement patterns of engineers within the factory
References


- Adam DC, Wu P, Wong JY, Lau EHY, Tsang TK, Cauchemez S, Leung GM, Cowling BJ. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat Med [Internet]. 2020 Sep 17 [cited 2023 Apr 27];26(11):1714-9. https://doi.org/10.1038/s41591-020-1092-0 Google Scholar
- Gong X, Xiao W, Cui Y, Wang Y, Kong D, Mao S, Zheng Y, Xiang L, Lu L, Jiang C, Yu X, Zhu Y, Fang Q, Pan H, Wu H. Three infection clusters related with potential pre-symptomatic transmission of coronavirus disease (COVID-19), Shanghai, China, January to February 2020. Eurosurveillance [Internet]. 2020 Aug 20 [cited 2023 Apr 27];25(33):pii=2000228. https://doi.org/10.2807/1560-7917.ES.2020.25.33.2000228 PubMed | Google Scholar
- Wilson E, Donovan CV, Campbell M, Chai T, Pittman K, Seña AC, Pettifor A, Weber DJ, Mallick A, Cope A, Porterfield DS, Pettigrew E, Moore Z. Multiple covid-19 clusters on a university campus – North Carolina, August 2020. MMWR Morb Mortal Wkly Rep [Internet]. 2020 Oct 2 [cited 2023 Apr 27];69(39):1416-8. https://doi.org/10.15585/mmwr.mm6939e3 PubMed | Google Scholar
- World Health Organization. Considerations in the investigation of cases and clusters of COVID-19: Interim guidance 22 October 2020 [Internet]. Geneva: World Health Organisation; 2020 Oct 22 [cited 2023 April 27]. 5 p. Document number.: WHO/2019-nCoV/cases_clusters_investigation/2020.3. Google Scholar
- Tejamaya M, Phanprsit W, Kim J, Tsai FJ, Muto G, Miller D, Reginald A, Granadillos N, Capule C, Zainal Farid MB, Lin Y wen, Park J, Chen RY, Lee KH, Park J, Hashimoto H, Kwon H, Yoon C, Padungtod C, Safira EA, Park DU. Characteristics of COVID-19 infection clusters occurring among workers in several Asia-Pacific countries. Ind Health [Internet]. 2022 Jan 12 [cited 2023 Apr 27];60(6):589-98. https://doi.org/10.2486/indhealth.2021-0227 PubMed | Google Scholar
- Al-Kuwari MG, Al-Nuaimi AA, Abdulmajeed J, Semaan S, Al-Romaihi HE, Kandy MC, Swamy S. COVID-19 infection across workplace settings in Qatar: a comparison of COVID-19 positivity rates of screened workers from March 1st until July 31st, 2020. J Occup Med Toxicol [Internet]. 2021 June 17 [cited 2023 Apr 27];16(1):21. https://doi.org/10.1186/s12995-021-00311-5 PubMed | Google Scholar
- Eurosurveillance Editorial Team. Updated rapid risk assessment from ECDC on coronavirus disease (COVID-19) pandemic in the EU/EEA and the UK: resurgence of cases. Eurosurveillance [Internet]. 2020 Aug 13 [cited 2023 Apr 27]; 25(32):pii=2008131. https://doi.org/10.2807/1560-7917.ES.2020.25.32.2008131 PubMed | Google Scholar
- Han J, Zhang X, He S, Jia P. Can the coronavirus disease be transmitted from food? A review of evidence, risks, policies and knowledge gaps. Environ Chem Lett [Internet]. 2020 Oct 1 [cited 2023 Apr 27];19(1):5-16. https://doi.org/10.1007/s10311-020-01101-x PubMed | Google Scholar
- Migisha R, Kwesiga B, Mirembe BB, Amanya G, Kabwama SN, Kadobera D, Bulage L, Nsereko G, Wadunde I, Tindyebwa T, Lubwama B, Kagirita AA, Kayiwa JT, Lutwama JJ, Boore AL, Harris JR, Bosa HK, Ario AR. Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches - March-April 2020. Global Health [Internet]. 2020 Nov 25 [cited 2023 Apr 27];16(1):114. https://doi.org/10.1186/s12992-020-00643-7 PubMed | Google Scholar
- MoH Uganda. COVID-19 Situation Report: SitRep 181 [Internet]. Kampala, Uganda: MoH; 2020 August 17 [cited 2023 April 27].
- Migisha R, Morukileng J, Biribawa C, Kadobera D, Kisambu J, Bulage L, Ndyabakira A, Katana E, Mills LA, Ario AR, Harris JR. Investigation of a covid-19 outbreak at a regional prison, Northern Uganda, September 2020. Pan Afr Med J [Internet]. 2022 Sep 6 [cited 2023 Apr 27];43(10). https://doi.org/10.11604/pamj.2022.43.10.33598 PubMed | Google Scholar
- Uganda Bureau of Statistics. Uganda´s District population projections 2015-2020. BUIKWE District Population Projection 2015-2020 [Internet]. Uganda: Data.Ug; 2017 Oct 13[cited 2023 Apr 27].
- Kelsey JL, editor. Methods in observational epidemiology. 2nd ed. New York: Oxford University Press; 1996. 432 p. (Monographs in epidemiology and biostatistics).
- Rahimi Z, Shirali GA, Araban M, Mohammadi M Javad, Cheraghian B. Mask use among pedestrians during the Covid-19 pandemic in Southwest Iran: an observational study on 10,440 people. BMC Public Health [Internet]. 2021 Jan 14 [cited 2023 Apr 27];21(1):133. https://doi.org/10.1186/s12889-020-10152-2 PubMed | Google Scholar
- Amir K. Covid-19- related stigma in covid-19 survivors in Kampala, Uganda: A qualitative study [Preprint]. 2021 Jan 19 [cited 2023 Apr 27]: [11p.]. https://doi.org/10.21203/rs.3.rs-150583/v1 Google Scholar
- Bukuluki P, Mwenyango H, Katongole SP, Sidhva D, Palattiyil G. The socio-economic and psychosocial impact of Covid-19 pandemic on urban refugees in Uganda. Social Sciences & Humanities Open [Internet]. 2020 July 23 [cited 2023 Apr 27];2(1): 100045. https://doi.org/10.1016/j.ssaho.2020.100045 PubMed | Google Scholar
- Ramesh N, Siddaiah A, Joseph B. Tackling corona virus disease 2019 (COVID 19) in workplaces. Indian Journal of Occupational and Environmental Medicine [Internet]. 2020 Mar 18 [cited 2023 Apr 27];24(1):16-18. https://doi.org/10.4103/ijoem.IJOEM_49_20 PubMed | Google Scholar
- Mboowa G, Musoke D, Bulafu D, Aruhomukama D. Face-masking, an acceptable protective measure against covid-19 in Ugandan high-risk groups. Am J Trop Med Hyg [Internet]. 2020 Dec 14 [cited 2023 Apr 27]; 104(2):502-513. https://doi.org/10.4269/ajtmh.20-1174 PubMed | Google Scholar
- Li T, Liu Y, Li M, Qian X, Dai SY. Mask or no mask for COVID-19: A public health and market study. PLoS ONE [Internet]. 2020 Aug 14 [cited 2023 Apr 27];15(8): e0237691. https://doi.org/10.1371/journal.pone.0237691 PubMed | Google Scholar
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, Chu DK, Akl EA, El-harakeh A, Bognanni A, Lotfi T, Loeb M, Hajizadeh A, Bak A, Izcovich A, Cuello-Garcia CA, Chen C, Harris DJ, Borowiack E, Chamseddine F, Schünemann F, Morgano GP, Muti Schünemann GEU, Chen G, Zhao H, Neumann I, Chan J, Khabsa J, Hneiny L, Harrison L, Smith M, Rizk N, Giorgi Rossi P, AbiHanna P, El-khoury R, Stalteri R, Baldeh T, Piggott T, Zhang Y, Saad Z, Khamis A, Reinap M, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet [Internet]. 2020 Jun 1 [cited 2023 Apr 27];395(10242):1973-87. https://doi.org/10.1016/S0140-6736(20)31142-9 PubMed | Google Scholar
- Rubin D, Huang J, Fisher BT, Gasparrini A, Tam V, Song L, Wang X, Kaufman J, Fitzpatrick K, Jain A, Griffis H, Crammer K, Morris J, Tasian G. Association of social distancing, population density, and temperature with the instantaneous reproduction number of sars-cov-2 in counties across the united states. JAMA Netw Open [Internet]. 2020 Jul 23 [cited 2023 Apr 27];3(7): e2016099. https://doi.org/10.1001/jamanetworkopen.2020.16099 PubMed | Google Scholar