SARS-CoV-2 Infection among Students at a High School, Mashonaland West, Zimbabwe, December, 2020
Nhidza Godwell1, Chirundu Daniel2, Govha Emmanuel1, Gombe Notion3, Juru Tsitsi Patience1,&, Tshimanga Mufuta1
1University of Zimbabwe, Family Medicine/Global and Public Health Unit, 2Kadoma City Health Department, 3African Field Epidemiology Network (AFENET)
&Corresponding author
Tsitsi Patience Juru, University of Zimbabwe, Family Medicine/Global and Public Health Unit, Zimbabwe. tsitsijuru@gmail.com
Introduction:
COVID-19 continues to be a major public health problem globally. On December 1, 2020, nine students at a high school presented at the school clinic with flu-like symptoms. COVID-19 was suspected and nasopharyngeal swabs were collected. The nine samples tested positive for SARS-CoV-2 on Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) test. From the first to the 8th of December 2020, the attack rate increased from 2.6% to 29.8%. We described the outbreak by person, place and time and determined factors associated with the outbreak at the school.
Methods:
We conducted a retrospective cohort study. A student or staff member at the school who had undergone RT-PCR, SARS-CoV-2 testing was recruited into the study. Data were collected using a pretested questionnaire, checklists and observations. Means, medians, frequencies, risk ratios, adjusted risk ratios and their corresponding 95% CI were calculated using Epi Info 7. We used the same software to construct an epidemic curve. We calculated student density in classrooms and dormitories and determined the relationship between student density and attack rates.
Results:
The overall COVID-19 attack rate among the 340 recruited participants was 31.8 %. Sharing utensils with a confirmed case (aRR=6.47, 95% CI: 2.97-14.1) and being in contact with a positive case within 1 metre in the past 7 days (aRR=17.2, 95% CI: 7.42-39.9) were independent risk factors associated with contracting SARS-CoV-2 infection. Owning and using a personal hand sanitizer (aRR=0.04, 95%CI: 0.02-0.10) and consistency in hand washing (aRR=0.16, 95%CI: 0.07-0.33) were protective factors. The mean student density was 2.8m2 (Min1.5, Max 3.0) classrooms and 3.1 m2 (Min 2.5, Max 3.9) in dormitories. There was a negative linear relationship between average bed spacing and attack rates of COVID-19 in hostels.
Conclusion:
Sharing of utensils or belongings and being in contact with a COVID- 19 case were risk factors for the outbreak. Overcrowding in the classrooms and dormitories fuelled the spread of the virus. We prohibited sharing of utensils, increased hand washing facilities with soap and reduction of the number of new intakes of form 1 and 5 students for 2021. Bed spacing in the dormitories was adjusted so that each student occupies the recommended 3.75m2/student.
Introduction

Coronaviruses are a family of contagious viruses [1,2]. They belong to the Coronaviridae family in the Nidovirales order [3]. Corona represents crown-like spikes on the outer surface hence the name [4]. The viruses contain a single-stranded Ribonucleic Acid (RNA) as nucleic material [4,5]. The subgroups of the coronavirus family are alpha (α), beta (β), gamma (γ), and delta (δ) [6]. Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2) belongs to the same group as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) viruses [7]. Corona viruses can mutate rapidly and form new variants. SARS-CoV-2 is the causative agent of Coronavirus disease of 2019 (COVID-19) pandemic [8]. COVID-19 symptoms include fever or chills, dry cough, tiredness, shortness of breath, respiratory distress and runny nose [9].
Tests for COVID-19 fall into two broad groups: tests that detect the presence of SARS-CoV-2 virus and tests that detect the presence of antibodies to SARS-CoV-2. Tests for the presence of virus usually use methods that recognize and amplify SARS-CoV-2 viral nucleic acid, such as reverse-transcriptase polymerase chain reaction (RT-PCR). Reverse transcription polymerase chain reaction (RT-PCR) is the gold standard for diagnosis of SARS-CoV-2 infection [
10,
11].
As of 1 December 2020, Zimbabwe had recorded 10 129 COVID-19 cases and 277 deaths. However, there was no published information on the risk factors in school going children [
12]. To mitigate spread of the COVID 19 pandemic, the Government of Zimbabwe formulated a COVID- 19 Emergency Response Plan. The plan focused on different pillars of coordination which included risk communication and community engagement, surveillance, case management, points of entry, infection prevention and control, logistics and continuity of health services [
13]. Further mitigation strategies included increasing the testing capacity, training of health workers on patient care, and increasing the number of quarantine and isolation centers [
14].
Due to the rising number of COVID 19 cases, the Zimbabwean authorities ordered closure of all schools from 24 March to 28 September 2020 so as to lessen the risk of students infecting each other [
13]. On the 25th August 2020 the Zimbabwean Ministry of Primary and Secondary Education (MOPSE) announced the reopening of schools in a phased approach where the exam classes (grade 7, form 4 and form 6) opened on the 28th of September 2020, followed by non-exam classes (grade 6, form 3 and form 5) who opened on the 26th of October 2020 and lastly the remaining classes which opened on the 9th of November 2020 [
14].
Sanyati Baptist High school also followed the phased opening approach as advised by the MOPSE and no cases of COVID -19 were reported until the 1st of December 2020, when nine female students presented at the school clinic with flu-like symptoms. The attending health workers suspected COVID-19 and collected nasopharyngeal swabs for SARS-CoV-2 RT-PCR testing. All the nine samples tested positive for SARS-CoV-2. The sister in charge (SIC) at the school clinic notified the District Medical Officer (DMO) about the suspected outbreak. On the same day the DMO notified the Provincial Medical Director (PMD) who in turn notified the epidemic and disease control directorate at the national office. From 1 to 8 December 2020, the COVID-19 attack rates increased from 2.6% to 29.8% respectively.
On the 2nd of December 2020 Sanyati district Rapid Response Team (RRT) visited the school for preliminary investigations. The RRT was given the printed copies of the laboratory results which confirmed that samples collected tested positive for SARS-CoV-2. The RRT collected 100 nasopharyngeal samples for testing from both students, non-teaching staff and teachers such that by the 6th of December 2020, thirty-four people had tested positive for COVID-19 at the school. The district hospital executive (DHE) and the headmaster of the high school requested the Kadoma city health department to carry out an outbreak investigation to describe the outbreak by person, place and time as well as to determine the factors associated with contracting SARS-CoV-2.
Methods


Study setting
We conducted the study at Sanyati Baptist High School in Sanyati District, Mashonaland West Province of Zimbabwe. Sanyati Baptist High School is a boarding school located 80 km due west of Kadoma City which is the capital for Mashonaland West Province. The responsible authority for the school is the Baptist Church in Zimbabwe. The school has an enrolment of 612 (485 boarders and 127 day-scholars) with form one up to six. There are 62 teaching and non-teaching staff. The school has eight dormitories, sixteen classrooms, one dining hall and one recreational hall. Students access health services at the school clinic.
Preliminary investigations and formulation of case definitions
We used the World Health Organization (WHO) case definitions to identify suspected cases. We defined a suspected case as a person who reported any three or more of the following signs or symptoms fever, cough, headache, shortness of breath, sore throat, sneezing, abdominal pain, chest pain and loss of smell or taste. We also defined a contact as an individual who has been in close contact within one meter with someone who had tested positive for COVID-19 with RT-PCR and a confirmed case as any person with laboratory confirmation of SARS-CoV-2 infection, irrespective of clinical signs and symptoms.
Case investigations
We constructed a line list of all positive cases to capture demographic data, epidemiological information on signs and symptoms, date of onset, age, class of students and type of employment for staff. We also collected information on any history of close contact with a confirmed case, observing prevention measures and sharing belongings in the hostels and classroom. All cases on the line list were interviewed including students, teaching and non-teaching staff. The primary case had onset of symptoms on 23 November 2020. She reported having met with her mother who had returned from South Africa seven days earlier. When she noticed some symptoms resembling infection with SARS CoV-2 she continued going to school and was not isolated. No contact tracing was done until the second of December when she tested positive with the other students who had reported symptoms at the school clinic. We also found that the primary case and her close contacts had contact with several other students and teaching staff hence we used the WHO case definitions to select those who we tested using the SARS-CoV-2 PCR test. We continued testing, case investigation, isolation and quarantining those waiting for results.
Descriptive epidemiology and hypothesis generation
We analyzed the data gathered from case investigations by time, place and person to generate a hypothesis for our investigation. Findings of our descriptive epidemiology suggested that all cases had a contact either at the dormitories or in class before the onset of illness. We also found that the majority of cases were sharing utensils (e.g., folks, spoons and plates) and belongings (e.g., combs, shoe brushes and even masks) at school and they were not wearing facemasks properly and consistently. From these findings, we hypothesized that sharing utensils or belongings was the likely risk factor for the outbreak.
Cohort study
Study design
We conducted a retrospective cohort study at Sanyati High School to test our hypothesis and determine other factors which were associated with the outbreak. We used a retrospective cohort design because the outbreak occurred at a boarding school with a defined population with the same characteristics. A cohort study design enabled us to calculate attack rates, relative risks and measures of impact for different categories. The cohort consisted of the students and teachers who were tested for SARS-CoV-2 at the school using RT-PCR after being screened using the WHO case definitions. The exposure was being exposed to the risk factors of contracting SARS-CoV-2 e.g., not wearing a face mask, not owning a personal hand sanitizer, not sanitizing consistently, not washing hands and not using foot baths at main entrances. Those not exposed to the risk factors of contracting SARS-CoV-2 e.g., wearing a face mask, owning a personal hand sanitizer, sanitizing consistently, washing hands and using footbaths at main entrances.
Study population and sampling
The study population were students and staff members at Sanyati Baptist High school. The study unit was any individual student or staff member who was tested for COVID-19 using RT-PCR. We included all students and staff members at Sanyati Baptist School who had undergone RT-PCR SARS-CoV-2 testing. Students and staff members who did not consent to participate in the study were excluded from the study.
We calculated a sample size of 384 using Fleiss formula embedded in epi info 7 at 95% CI and 80% power based on a study by Ng et.al. (2020), who reported an association between sharing a bedroom with a confirmed case and contracting COVID-19 [
15]. We recruited all the students and staff members who underwent RT-PCR testing and gave consent to participate in the study.
Data collection
We collected data using a pretested interviewer administered questionnaire, key informant interviews (headmaster, sister in charge at the school clinic, matron and boarding master) and check lists. The interviewer administered questionnaire was used to capture information on demographic characteristics of respondents (age, sex, class, form, hostel), signs and symptoms (headache, loss of smell, shortness of breath, sneezing, rash, abdominal pain and diarrhea) of COVID 19 among cases and factors associated with contracting COVID 19 which included sharing utensils, lack of knowledge of COVID-19 and not maintaining social distance. The same questionnaire was also used to collect information on the following knowledge attributes: how COVID-19 is spread, what is the causative agent of COVID 19, signs and symptoms of COVID 19 and prevention measures of COVID 19. The questionnaire was administered to students and staff (teaching and non-teaching staff).
We used a checklist to collect information on school enrolment, number of students in each class, number of students in each hostel, the presence of footbaths at main entrances and handwashing facilities. We also used the same tool to collect information on hostels floor areas and average bed spacing as well as number and size of windows in the dormitories and classrooms.
We used a checklist adopted from the Integrated Disease Surveillance and Response Technical Guidelines (IDSR) third edition 2019 to assess outbreak preparedness and response for Sanyati District. [
16]. We collected data on availability of outbreak emergency kit, a rapid response team and an emergency preparedness response plan (EPR).
Permission to carry out the study was sought and obtained from school authorities and Kadoma City directorate. Written informed ascent from the school going children and consent from adults were obtained respondents.
Data analysis
Data were captured and analyzed using Epi Info 7.2.4.0™ (CDC, 2020) statistical software. An electronic questionnaire was created in the software. Data were entered, cleaned for transcription errors, missing details, duplicate information and values that were out of range. Quantitative data was analyzed using Epi Info and qualitative data was analyzed thematically. The software was used to generate medians, frequencies, confidence intervals, p values and proportions on univariate analysis. Relative risks were also generated on bivariate analysis. Backward multivariate logistic regression was done to identify independent factors associated with the outbreak as measured by the adjusted relative risks and p values. The significance level was set at 5% and a 95% confidence interval was used. The epi-curve was generated using Microsoft office (2016) with the date of onset of symptoms and number of cases. The spot map was generated using google maps. Knowledge was assessed using a 3-point Likert scale were those who answered 0-2 knowledge attributes correctly were regarded as having poor knowledge and those who answered 3-5 attributes correctly were knowledgeable. We calculated dormitory-student and classroom-student ratio and compared it to the standard ratios approved by the Government of Zimbabwe to assess overcrowding. Any density higher than 3.50m2/student in classroom and 3.75m²/student in hostels was regarded as overcrowding.
Availability of data and material
The data that support the findings of this study are available from Ministry of Health and Child Care (Zimbabwe) but restrictions apply to the availability of these data. Data are however available from the authors upon reasonable requests and with permission of Ministry of Health and Child Care (Zimbabwe).
Ethical considerations
Permission to proceed with the study was obtained from the Institutional Review Board Kadoma City, University of Zimbabwe, School authorities and Department of Primary Health Care Services.
Results


Descriptive epidemiology
Demographic characteristics of study participants at Sanyati Baptist High school, December 2020
We recruited and interviewed all the 340 participants who underwent SARS-COV-2 PCR testing. Out of the 340 participants, the majority 175 (51%) were females and 123 (37%) were from form four class. The form fives contributed the least number 13 (4%) of participants. The majority 327(97%) were in boarding and 355(98%) were students. The median age of respondents was 16 years (Q1=14; Q3=17)
Table 1.
Description of outbreak by person at Sanyati Baptist high school, December, 2020
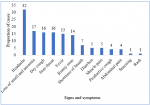
Out of the 340 who were tested for SARS-CoV-2, 140 (41%) tested positive and 136 (97%) of the 140 were symptomatic. Among the symptomatic cases, the majority 105 (77%) were females. The commonly reported signs and symptoms were headache 107(32%), loss of taste or anosmia 58(17%) whilst two (1%) and four (1%) reported rash and sneezing respectively
Figure 1. Three quarters of the cases were from the 15-20 years age group. All cases were isolated within the school premises. Severe cases were managed with azithromycin 10 (7%) and paracetamol 8(6%). All the cases recovered with a median recovery time of 14 days (Q1=7; Q3=17).
Description of the outbreak by place at Sanyati Baptist high school, December 2020
The majority of cases were from Ingwe boys´ hostel 23 (58%), and Nyati boys´ hostel 20(50%). The least number of cases were recorded in Mbizi and Kamba hostels with 4% each. In the girls hostels the highest number of cases were recorded in Cheetahs girls´ hostel 47 (91%), followed by Chipembere girls´ hostel with 30 (55%). The least number of cases was in Lion girls´ hostel with 5(14%)
Figure 2.
Description of outbreak by time at Sanyati Baptist high school, December 2020
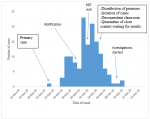
The primary case exhibited initial symptoms on 23 November 2020. The first case was notified on the 1st of December 2020. The Rapid Response Team (RRT) visited the school on the 2nd of December 2020 and control measures, which included disinfection of premises, isolation of cases, quarantine of close contacts waiting for results and sending home those who had negative results were put in place. Based on the epicurve, and using the date of onset the number of cases increased from one on the 26th of November 2020 to 10 in 24 hours reaching a peak of 23 cases on the 1st of December 2020. The peaks became progressively taller from the 27th of November 2020 with two more peaks recorded on the 1st and 3rd of December 2020. The last case was reported on the 11th of December 2020. From the 3rd of December 2020, there was a sharp decline in the number of cases. The outbreak duration was 17 days. The curve demonstrated a propagated type of disease spread
Figure 3.
Analytical epidemiology
Factors associated with contracting SARS-CoV-2 virus
Significant protective factors against contracting SARS-CoV-2 infection were possession and consistent use of a personal hand sanitizer (RR 0.22; C.I. 0.16-0.31), consistency in handwashing (RR=0.23; C.I.0.44-0.97), use of footbaths at main entrances (RR=0.26; C.I.0.22-0.97), having received health education on COVID-19 (RR=0.41; C.I.0.34-0.49) and use of soap and water for handwashing (RR=0.48; C.I.0.44-0.97).
Sharing a hostel with someone exhibiting COVID-19 symptoms (RR =4.24; C.I.2. 44-5.56) and sharing a classroom with a SAR-CoV-2 positive person (RR=1.89; C.I.1.33-2.69), sharing utensils or belongings with a confirmed COVID-19 case (RR=2.60; C.I.1.96-3. 47), and being in contact with a positive case within 1m in the past 7 days (RR=5.5; C.I.3. 48-8.72) were found to be risk factors for contracting SARS-CoV 2.
Sharing utensils or belongings with a confirmed case (aRR=6.47, 95% CI: 2.97-14.10) and being in contact with a positive case within 1m in the past 7 days (aRR=17.23,95% CI: 7.42-39.99) were independent risk factors associated with contracting SARS-CoV-2 infection. Possession and consistent use of a personal hand sanitizer (aRR=0.04, 95%CI: 0.02-0.10) and consistency in hand washing with soap and water (aRR=0.16, 95%CI: 0.07-0.33) were independent protective factors against contracting SARS-CoV-2 infection
Table 2.
Measures of Impact
The excess risk of SARS-CoV-2 infection among those who shared utensils or belongings with a confirmed COVID-19 case was 38 per 100. About 61.5% of SARS-CoV-2 infection among those who shared utensils or belongings with a confirmed COVID-19 case could be attributed to sharing utensils or belongings with a COVID-19 confirmed case, and could be eliminated if students had not shared utensils or belongs with a confirmed COVID-19 case.
The excess risk of infection with SARS-CoV-2 among those who were in contact with a confirmed COVID-19 case within 1 m in the past 7 days was 52 per 100. Approximately 81.3% of SARS-CoV-2 among those who reported being in contact with a confirmed COVDI-19 case within 1m in the past 7 days can be attributed to close contact of within 1 m with a confirmed case and could be eliminated if had not been in close contact within 1 m with a confirmed case
Table 3.
Environmental assessment at Sanyati Baptist high school, December 2020
The school facilities had footbaths with 2% sodium hypochlorite at all main entrances and hand washing facilities with water and soap in every class and hostel. According to the modern building bylaws each student should occupy an area of 3.5m2 in classrooms, and 3.75m2 in the hostels however, at Sanyati Baptist high school the mean areas occupied by a student in classrooms was 2.8m2 (Min1.5, Max 3.0) and 3.5m2 (Min 2.5, Max 3.9) in the hostels. There was a significant positive correlation between attack rates and the number of students per hostel (r=0.84, R2=0.72). There was a negative correlation between the attack rate of COVID-19 and day light ventilation area (area of the window through which sunlight can pass through) (r=-0.53, R2=0.28).
Evaluation of outbreak preparedness, detection and response at Sanyati Baptist high school, December 2020
Sanyati district´s RRT was made up of an Environmental Health Practitioner, clinician, laboratory technician, Environmental Health Officer, and Public Health Officer. The district had an outbreak emergency kit that could cater for 100 SARS-CoV-2 infected patients. The emergency outbreak kit comprised of medicines (azithromycin, paracetamol) N95 facemasks, gloves, swabs to collect 100 patients and Typex Suits. The COVID-19 management guidelines were available at Sanyati Baptist School Clinic (the local clinic). Two of the four nurses at the local clinic were trained in Integrated Disease Surveillance and Response (IDSR). Emergency Prepared and Response meetings had been held for each quarter as evidenced by the presence of minutes of the meetings. During the outbreak the team also managed to hold meetings on a daily bases to update on the progress and control of the outbreak. The district RRT was notified of the outbreak on the 1st of December 2020 and the RRT visited the school within 24 hours. The RRT collected nasopharyngeal samples, isolated cases, and quarantined close contacts who were waiting for results. Health education on COVID-19 was given to all the students and teachers.
Discussion


In our study, we found that sharing utensils and belongings with a confirmed SARS-CoV-2 case was independently associated with contracting the infection. This could be attributed to the ability of the SARS-CoV-2 to survive on surfaces for up to three to seven hours on hard surfaces, plastic and copper [17,18]. The majority of cases reported that they were sharing utensils, which include cups, spoons, folks and plates and these have been proven to be transmission vehicles if preventive measures were not observed. This is consistent with findings by Ng et.al. (2020) in Singapore who reported that sharing utensils was significantly associated with high transmission rates [19].
Consistent washing of hands with soap and water as well as owning and consistently using a hand sanitizer were found to be a protective factor. This was made possible by the presence of multiple hand washing facilities at the school. This finding was biologically plausible because the combined action of soap and water as well as use of alcohol-based sanitizers are known to effectively deactivate the virus [
20,
21]. Similar findings were reported in Thailand were frequent hand washing, was independently associated with lower risk for infection [
15].
In our study the majority of our cases were symptomatic. This could be attributed to a long-time lag between the first case and identification of the outbreak. This means the majority of our cases could have passed the pre symptomatic phase of the disease. These same findings were reported in Thailand where only four percent were asymptomatic [
19]. The most common symptoms among cases were headache, loss of taste or anosmia, dry cough, sore throat and fever. This finding can be explained by the nature of study participants who were mainly teenagers were fever is common due to their physiology [
18]. Regardless of differences in climates and geographical location, a study in China reported the same [
22].
Being in close contact within one meter with a confirmed case of SARS-CoV-2 increased the risk of contracting the infection by seventeen times. This was buttressed by the overcrowding which was found in the hostels and classrooms. Additionally, there was a positive correlation between the attack rate and hostel size-student ratio. As the number of students in the hostel increased, social distancing became difficult to maintain and this increased the chances of human-to-human infection through droplet infection. This is consistent with findings from Canada where people who were living in overcrowded housing were two times more likely to test positive for SARS-CoV-2 [
23]. We also found that the there was a negative correlation between the attack rates of COVID-19 and day light ventilation. Day light ventilation introduces ultraviolet radiation, which by its absorptive and photochemical effects damage the nucleic acid and hence disrupting the viral replication thereby inactivating the SARS CoV-2 virus [
24].
In this study, being knowledgeable on COVID-19 was found to be a protective factor against contracting SARS-CoV-2. This is because those who have good knowledge were more likely to practise safer prevention and control measures for COVID-19 than those who were not knowledgeable. Lorfa et.al. (2020) in Nigeria, reported that having adequate knowledge on COVID-19 was linked to lower risk of infection by SARS-CoV-2 [
25].
Our study added information on the transmission dynamics of the disease at a school setup. It gives evidence-based mitigations that can be done to curb the spread of the infection if an outbreak occurs in a school setup. It also provides control measures to put in place to prevent a similar outbreak in a school setting.
Limitations
The study may have been affected by recall bias since the analytical study started ten days later. The study might have been affected by social desirability bias but we tried to address it by also observing when assessing owning hand sanitizer, owning a face mask and use of footbaths at entrances.
Conclusion


Failure to maintain the recommended social distance in classrooms and hostels and sharing of utensils were associated with contracting the SARS-CoV 2 infection. Consistence in handwashing, owning a personal hand sanitizer and consistently using it and being knowledgeable on COVID-19 help reduce the transmission of SARS-CoV 2 infection among students. We prohibited sharing of utensils, increased hand washing facilities with soap and reduction of number of new intakes of form 1 and 5 students for 2021. Bed spacing in the dormitories was adjusted so that each student occupies the recommended 3.75m2/student. We, gave health education, provided psycho-social support, facemasks, hand sanitizers and we disinfected the premises.
What is known about this topic
- The causative agent of the disease and how it is spread in the communities and hospitals. The signs and symptoms, recovery rates as well as control measures
What this study adds
- Our study added information on the transmission dynamics of the disease at a school setup. It gives evidence-based mitigations that can be done to curb the spread of the infection if an outbreak occurs in a school setup
- It also provides control measures to put in place to prevent a similar outbreak in a school setting.
Competing interests


The authors declare no competing interests.
Funding
This study was funded by Kadoma City Council and Health Studies Office.
Authors' contributions


GN, DC and EG: conception, design, acquisition, data collection, analysis and interpretation of data. GN and DC wrote the first draft of the manuscript. EG, NG, TJ and MT critically revised the draft for important intellectual content. All authors read and approved the final manuscript.
Acknowledgements


We would like to acknowledge Kadoma City, Health studies office, Ministry of Health and child care and Ministry of Primary and Secondary education.
Tables and figures


Table 1: Demographic Characteristics of Respondents at Sanyati Baptist High School, December, 2021
Table 2: Factors Associated with Contracting SARS-CoV-2 at Sanyati December, 2020.
Table 3: Measures of Impact at Sanyati Baptist High School, December, 2020
Figure 1: Presenting signs and symptoms COVID-19 at Sanyati High school, December 2020
Figure 2: The Spot maps showing Attack Rates hostel, at Sanyati High school, December 2020
Figure 3: Epidemic curve for COVID-19 at Sanyati High school, December 2020
References


- National Foundation for Infectious Diseases. Coronaviruses. National Foundation for Infectious Diseases. 2020. Accessed Dec 2020.
- American Lung Association. Coronavirus (CoV). American Lung Association. 2020. Accessed Dec 2020.
- Zhou Z, Qiu Y, Ge X. The taxonomy, host range and pathogenicity of coronaviruses and other viruses in the Nidovirales order. Anim Dis. 2021; 1(1):5.https://doi.org/10.1186/s44149-021-00005-9 PubMed | Google Scholar
- Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020 Mar 16; 24:91-98.https://doi.org/10.1016/j.jare.2020.03.005 PubMed | Google Scholar
- Ouassou H, Kharchoufa L, Bouhrim M, Daoudi NE, Imtara H, Bencheikh N, ELbouzidi A, Bnouham M. The Pathogenesis of Coronavirus Disease 2019 (COVID-19): Evaluation and Prevention. J Immunol Res. 2020 Jul 10; 2020:1357983.https://doi.org/10.1155/2020/1357983 PubMed | Google Scholar
- Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018 Feb; 23(2):130-137. https://doi.org/10.1111/resp.13196 PubMed | Google Scholar
- NIH: National Institute of Allergy and Infectious Diseases. Coronaviruses. NIH: National Institute of Allergy and Infectious Diseases. 2020. Accessed Dec 2020.
- Jiang S, Shi Z, Shu Y, Song J, Gao GF, Tan W. A distinct name is needed for the new coronavirus. The Lancet. 2020 Mar 21; 395(10228):949.https://doi.org/10.1016/S0140-6736(20)30419-0 . PubMed | Google Scholar
- Neamah SR. Comparison between symptoms of COVID-19 and other respiratory diseases. Electronic Journal of Medical and Educational Technologies. 2020 Aug 29; 13(3):em2014. https://doi.org/10.30935/ejmets/8489. Google Scholar
- Kumar R, Nagpal S, Kaushik S, Mendiratta S. COVID-19 diagnostic approaches: different roads to the same destination. Virusdisease. 2020 Jun; 31(2):97-105. https://doi.org/10.1007/s13337-020-00599-7 PubMed | Google Scholar
- World Health Organization (WHO). Novel coronavirus (COVID-19). 2020. Accessed December 2020.
- Zimbabwe Ministry of Health and Child Care. COVID-19: situation report. Zimbabwe: Ministry of Health and Child Care. Accessed December 2020.
- Zimbabwe Ministry of Health and Child Care. Covid 19 Pillars. Zimbabwe: Ministry of Health and Child Care. Accessed December 2020.
- Murewanhema G, Burukai T, Mazingi D, Maunganidze F, Mufunda J, Munodawafa D, Pote W. A descriptive study of the trends of COVID-19 in Zimbabwe from March-June 2020: policy and strategy implications. Pan Afr Med J. 2020 Nov 9; 37(Suppl 1):33.https://doi.org/10.11604/pamj.supp.2020.37.33.25835 PubMed | Google Scholar
- Ng OT, Marimuthu K, Koh V, Pang J, Linn KZ, Sun J, De Wang L, Chia WN, Tiu C, Chan M, Ling LM, Vasoo S, Abdad MY, Chia PY, Lee TH, Lin RJ, Sadarangani SP, Chen MI, Said Z, Kurupatham L, Pung R, Wang LF, Cook AR, Leo YS, Lee VJ. SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study. Lancet Infect Dis. 2021 Mar; 21(3):333-343.https://doi.org/10.1016/S1473-3099(20)30833-1 PubMed | Google Scholar
- WHO. The World Health Organisation, third edition of the Integrated Disease Surveillance and Response Technical Guidelines. WHO. Accessed Jan 2021.
- Nishiura H, Linton NM, Akhmetzhanov AR. Initial Cluster of Novel Coronavirus (2019-nCoV) Infections in Wuhan, China Is Consistent with Substantial Human-to-Human Transmission. J Clin Med. 2020 Feb 11;9(2):488. https://doi.org/10.3390/jcm9020488 PubMed | Google Scholar
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annual review of virology. 2020 Sep 29; 7:83-101.https://doi.org/10.1146/annurev-virology-012420-022445 . Google Scholar
- Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, Eungkanit N, Pisitpayat N, Srisong N, Yasopa O, Plernprom P, Promduangsi P, Kumphon P, Suangtho P, Watakulsin P, Chaiya S, Kripattanapong S, Chantian T, Bloss E, Namwat C, Limmathurotsakul D. Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. Emerg Infect Dis. 2020 Nov;26(11):2607-2616.https://doi.org/10.3201/eid2611.203003 PubMed | Google Scholar
- Türsen Ü, Türsen B, Lotti T. Coronavirus-days in dermatology. Dermatol Ther. 2020 Jul; 33(4):e13438.https://doi.org/10.1111/dth.13438 PubMed | Google Scholar
- Dehbandi R, Zazouli MA. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020 Aug 1; 1(4):e145. https://doi.org/10.1016/S2666-5247(20)30003-3. Google Scholar
- Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, Chen H, Wang D, Liu N, Liu D, Chen G, Zhang Y, Li D, Li J, Lian H, Niu S, Zhang L, Zhang J. Characteristics of COVID-19 infection in Beijing. J Infect. 2020 Apr; 80(4):401-406. https://doi.org/10.1016/j.jinf.2020.02.018 PubMed | Google Scholar
- Sundaram ME, Calzavara A, Mishra S, Kustra R, Chan AK, Hamilton MA, Djebli M, Rosella LC, Watson T, Chen H, Chen B. The individual and social determinants of COVID-19 diagnosis in Ontario, Canada: A population-wide study.https://doi.org/10.1101/2020.11.09.20223792 . Google Scholar
- Storm N, McKay LGA, Downs SN, Johnson RI, Birru D, de Samber M, Willaert W, Cennini G, Griffiths A. Rapid and complete inactivation of SARS-CoV-2 by ultraviolet-C irradiation. Sci Rep. 2020 Dec 30; 10(1):22421. https://doi.org/10.1038/s41598-020-79600-8 PubMed | Google Scholar
- Iorfa SK, Ottu IFA, Oguntayo R, Ayandele O, Kolawole SO, Gandi JC, Dangiwa AL, Olapegba PO. COVID-19 Knowledge, Risk Perception, and Precautionary Behavior Among Nigerians: A Moderated Mediation Approach. Front Psychol. 2020 Nov 20; 11:566773. https://doi.org/10.3389/fpsyg.2020.566773 PubMed | Google Scholar