A descriptive study of a SARS-CoV-2 super spreader event: A funeral and a house-party in a district municipality of the Eastern Cape Province, South Africa, 2020
Phuti Sekwadi1,&, Nomlindo Makubalo2, Ntathu Mini2, Lifukazi Ngcwangu2, Mzimasi Neti1, Ahmad Haeri Mazanderani1,3, Nevashan Govender1
1National Institute for Communicable Diseases, Private Bag X4, Sandringham, Johannesburg, 2131, South Africa, 2Nelson Mandela Bay Metropolitan, Eastern Cape Province, 3University of Limpopo, Limpopo Province, South Africa
&Corresponding author
Phuti Sekwadi, National Institute for Communicable Diseases, Private Bag X4, Sandringham, Johannesburg, 2131, South Africa. pgsekwadi@gmail.com
Introduction:
Coronavirus Disease 2019 (COVID-19) is a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). According to the World Health Organisation, modes of transmission for SARS-CoV-2 include contact, droplet and airborne transmission has also been reported. On 16 March 2020, Nelson Mandela Bay District in the Eastern Cape Province recorded its first case of SARS-CoV-2, which was travel related. On 21 March 2020, over 1000 people attended a funeral of a healthcare worker in one of the townships within the district. This study aims to quantify the incident infections associated with a single funeral and describe the chain of transmission.
Methods:
This is a retrospective descriptive study that uses COVID-19 data collected between March and April 2020 in Nelson Mandela Bay district. Interviews were conducted with newly reported COVID-19 cases by healthcare professionals through telephonic platforms and face-to-face. Data obtained through the interviews included possible exposures, risk factors, and demographics. Data analysis was done using Microsoft Excel.
Results:
Four-hundred-and-twelve cases of COVID-19 were reported within the district during the study period. Of the first 100 cases reported within the district, 42% (42/100) were linked to the funeral; these included people who attended the funeral and those who had contact with the funeral attendees.
Conclusion:
While funerals cannot be avoided, adherence to COVID-19 guidelines on funerals can help reduce infection transmission rates. Platforms such as virtual
funeral services and virtual memorial services can help reduce the risk of COVID-19 transmission associated with these types of events.
Introduction

Coronavirus Disease 2019 (COVID-19) is a respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 cases were first observed among dealers and vendors at a seafood, poultry, and live wildlife market in Wuhan, located within the Jianghan District of Hubei Province in China. The source of the virus is not yet known [1]. Some of the most common symptoms of this respiratory illness include fever, cough, and fatigue [2]. Recent studies have shown that loss of taste and loss of smell are characteristic symptoms of SARS-CoV-2 infection [3]. The median incubation period has been reported to be 5.1 days (95% CI, 4.5 to 5.8 days) [4]. While most people may never develop any symptoms, SARS-CoV-2 infection can lead to severe illness or death [5]. According to the World Health Organisation (WHO), there several modes of transmission for SARS-CoV-2 which include contact with an infected person, contact with droplets from an infected person and airborne transmission has also been reported [5]. The highest viral load has been reported among patients on the day of symptom onset and then a gradual decline in viral load noted thereafter; this correlates with the period when patients are most infectious [6, 7].
Prevention of new SARS-CoV-2 infection is a critical component of the response to the pandemic, which has rapidly spread across the world. The most important methods for curbing the spread of infection are isolation of the confirmed cases and quarantining of people who may have been exposed or in contact with a confirmed case [
8-10]. Since asymptomatic cases can also spread the infection, physical distancing becomes critical for everyone in the community [
11]. Physical distancing has been reported to reduce infection rates, as determined by a comparison of infection rates between countries that implemented and those that did not implement physical distancing measures [
12].
In this study, we look at the role of social events that sparked a chain of transmission in one district in the Eastern Cape Province, namely Nelson Mandela Bay. The study focuses on a funeral service that was conducted in the early days of the pandemic in the province, and within one week of the first confirmed SARS-CoV-2 case in the district. This study aims to add to the growing body of knowledge on SARS-CoV-2 and how it is transmitted and to make recommendations for curbing the spread of this novel coronavirus.
Methods


Study design
This is a retrospective descriptive study of the COVID-19 super spreader events identified in the Nelson Mandela Bay district between 16 March and 30 April 2020. The events include two earliest clusters of COVID-19 cases in the district.
In this study, a COVID-19 case is defined as any person with a confirmed laboratory diagnosis of SARS-CoV-2 during the study period. A contact is defined as any person who had prolonged close contact (>15min duration within 1.5 metre distance in a closed environment) with a confirmed case, even though they may not be sick themselves.
A COVID-19 cluster in this study is defined as five or more cases of laboratory-confirmed COVID-19 that have an epidemiological link.
Study setting
This study focuses on the Nelson Mandela Bay district in the Eastern Cape Province, which comprises seven other district municipalities. According to the 2007 census, the district had an estimated population of 1,050,930 with a median age of 26 years and the average household size was reported to be four people per household. The district is divided into three sub-districts, namely Sub-District A, B, and C.
On 16 March 2020, the district recorded its first case of SARS-CoV-2, which was a patient with recent international travel history to countries that had reported SARS-CoV-2 transmission. Due to the ongoing increase in the number of COVID-19 cases worldwide and within South Africa, the South African president declared a national state of disaster on 15 March 2020, and subsequently introduced the national lockdown on 26 March 2020, putting in place regulations to curb the spread of infection. Among these regulations were limitations on the number of people allowed to attend social gatherings including funeral and religious events, which were restricted to 50 people [
13].
However, on 21 March 2020, there was a funeral in one of the townships within the district. It was a burial of a healthcare worker, who worked as a nurse at one of the local clinics. The healthcare worker died from causes other than SARS-CoV-2. The funeral attracted more than a thousand attendees, which included family members, healthcare workers, and members of the community. As of the date of the funeral, only one case of confirmed SARS-CoV-2 had been reported within the district (on 16 March), which was travel related. This was the only case reported for the entire province as well.
Sample size
We included all the COVID-19 cases that were reported within the district between 16 March and 30 April 2020 because our focus is on the first clusters of cases identified in the district. The total number of people who attended the two events is unknown, as there were no attendance registers that were kept at these events. Only people who contracted COVID-19 after attendance of these events and had a positive COVID-19 test were included in this study. The sampling frame in both clusters was not available.
During the study period, SARS-CoV-2 testing criteria in South Africa was limited to hospitalized patients with severe acute respiratory illness and absence of an alternative diagnosis, and non-hospitalized patients with acute respiratory illness (defined as sudden onset of cough, sore throat, shortness of breath or fever) and a history of close contact with a COVID-19 case, travel outside of South Africa, or worked in or attended a health care facility where patients with SARS-CoV-2 infections were being treated 14 days prior to symptom onset. Asymptomatic contacts were not routinely tested at this stage.
Data collection
All the COVID-19 cases were diagnosed from both public and private laboratories that submit all the cases to a central database managed by the National Health Laboratory Service (NHLS). We obtained our data from the NHLS. A team of healthcare professionals followed up on the new cases within the district daily and conducted telephonic and/or face-to-face interviews with the cases. The interviews were done to gather possible exposures, risk factors, and demographics and more importantly to identify contacts to allow efficient contact tracing, testing, and facilitation of quarantine and isolation. A template of the questionnaire is available as an additional file (See additional file 1).
Data analysis
Data were captured and managed on google sheets (Google LLC. Data) and exported to Microsoft Excel. The analysis was done using Microsoft Excel to generate a Venn diagram showing different clusters identified and a histogram to display the epidemic curve. Age, gender, and outcome distributions were displayed using bar graphs generated through Microsoft Excel.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical considerations
The authors declare that all activities contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. NICD outbreak investigations are approved by the research ethics committee at the University of the Witwatersrand, Johannesburg, South Africa (Clearance certificate number: M160667).
Results


Descriptive epidemiology
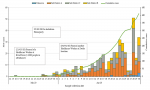
As of 30 April 2020, 412 laboratory-confirmed cases of COVID-19 had been reported from the public and private laboratories within the district. Sub-District C accounted for most of the cases at 43% (177/412) followed by Sub-District A and B with 42% (171/412) and 14% (56/412), respectively
Figure 1. The majority of these were female at 66% (272/412) and most cases were within age groups 25-29, 30-34, and 35-39 years with each accounting for 11% of the total cases
Figure 2. The median age was 38 years with a range of 0 to 87 years. Age groups 75-79 years and ≥80 years accounted for the least number of cases at 1% (5/412) each followed by children aged 0-4 years at 2% (8/412). Where symptom information was recorded (56%; 231/412), most of the cases were symptomatic (74%; 172/231). As of 30 April 2020, the highest death rates were observed within older age groups which include 80 years & above (20%), 75-79 years (20%), and 65-69 years (17%)
Figure 3.
Cluster description
There were two important clusters identified during the early stages of the pandemic in the district; these included a funeral gathering/service and a house party.
Funeral
A funeral took place on 21 March 2020 in Suburb A within Sub-District C. It was the funeral of a healthcare worker where there were reportedly over 1000 people in attendance.
There are different ways in which communities deal with grief across the globe. In South Africa, when death occurs in a family, the burial usually takes place a week after the passing on of the deceased. During this period people start gathering in that particular household to console family members and relatives who would be gathered in the household for the days leading to the day of the funeral. It is a norm that meals would be served to every visitor who comes to the house. Different visitors would be coming and going throughout this period.
African funerals are events usually rich with religious significance and practice. In every funeral, religion is practiced as a way of comforting the bereaved and conducting the funeral procession. This may include having a night vigil of singing and dancing as a way to comfort the bereaved, performing rituals by family members with the help of traditional healers, sharing meals, and many other practices, which involve close contact between people in mourning.
Houseparty
On 25 March 2020, (the eve of the national lockdown) a house-party was held in a household in Sub-District C. The attendees included individuals from other districts and other provinces, as the event occurred before the national lockdown, and the movement of people was not yet prohibited. Six of the attendees later tested positive for SARS-CoV-2 and one of these had close contact with an employee at Grocery store B. A chain of transmission among the employees of Grocery store B followed thereafter. This subsequently led to other clusters
Figure 4.
A total of 116 (28%; 116/412) of the cases reported close contact with a known case before illness onset. Of the total cases, 204 (50%; 204/412) could be linked to a specific cluster. The first two clusters that were identified included one associated with the funeral and the other associated with the house party
Figure 4. Of the first 100 cases, 42% (42/100) were linked to the funeral; these included people who attended the funeral and those who had contact with the funeral attendees.
Discussion


Contrary to what has been reported in other countries, including the United States where most of the cases were older (median of 43 years) during the same period as our study, most of the cases in South Africa were youths with the median age of 38 years [14-17]. There were more females than there were males, as shown in other studies [18, 19]. Some of the reasons for this could be poor health-seeking behavior among males [20]; and females more likely to be caregivers to those that are sick, increasing their risk of exposure. Fatality rates were higher among older age groups, which is in keeping with what has been reported in other countries [21-23].
Most of the cases in the early stages of the outbreak were linked to the funeral, with over 40% of the first 100 cases linked to the funeral. This could be an underestimate as people started to refrain from disclosing that they attended the funeral for fear of victimization. From the data available, this particular funeral was a SARS-CoV-2 super spreader event, and likely triggered a rapid and sustained chain of transmission of the virus within the district.
The testing guidelines at the time contributed to the majority of laboratory confirmed cases being symptomatic, as asymptomatic contacts were not routinely tested. Asymptomatic contacts were tested when they were part of a specific cluster, or for any other reason the testing personnel saw fit to have them tested. Lack of routine testing asymptomatic contacts may have also facilitated further community transmission, especially at social gatherings such as funerals, as contacts may not have heeded quarantine regulations if they were not feeling ill. Routine testing for asymptomatic contacts could help with case finding, timely patient isolation, and reducing the risk of further transmission. However, a shortage of COVID-19 testing kits at the time, led to prioritization of at-risk-groups for testing. A study looking at transmission rates between symptomatic and asymptomatic COVID-19 cases reported that asymptomatic cases accounted for more than 50% of all transmissions[
24]. Identification and isolation of asymptomatic cases are critical in reducing transmission rates [
25,
26].
Social gatherings are high-risk events for SARS-CoV-2 transmission [
27,
28]. Some of the COVID-19 super-spreader events realized earlier on in the South African context were funerals and religious gatherings [
29,
30]. These continue to be high risk. One religious event in the Free State Province was linked to 45% (44/97) of the cases reported in that province on 13 April 2020. The Eastern Cape Province has been one of the provinces with a high number of cases linked to funeral gatherings, with the province later became a COVID-19 hotspot in the country [
29,
31]. Studies from other countries have also shown the risk of SARS-CoV-2 transmission associated with religious/church gatherings [
32-34]. If indeed one has to attend any gathering all precautions necessary to prevent SARS-CoV-2 infection, transmission should be taken, and adherence to COVID-19 prevention measures should be of utmost importance.
Adherence to the COVID-19 funeral guidelines as issued by the government can help reduce infection transmission rates at these events. The guidelines include restricting funeral attendance to a small number of people (50 people or less during the study period). Maintaining physical distancing and wearing a mask all the time when attending a funeral. Cultural and religious practices remain important parts of South Africans´ lives; however, practices that expose people to this virus should be avoided and other less risky methods should be implemented. Virtual platforms can be used for events such as memorial services and funeral services to allow more people to offer their support and condolence during times of grief without having to congregate in large numbers. Studies have reported on how virtual platforms can enable more people to offer their support to bereaved families [
35,
36].
Community engagement in the form of mass public health educational campaigns, engagement of religious leaders in educating their constituents, and employing other community-based interventions can help improve adherence to existing COVID-19 prevention measures and guidelines by the public [
37-39]. The acceptance and adherence to COVID-19 prevention guidelines by communities in events such as funerals, which cannot always be policed, are critical in the response to the pandemic.
Major limitations in this study included a lack of complete data on the risk factors associated with infection and comorbidities among those who were infected and those who demised. Hence, conducting an analytical study was not feasible. However, from the descriptive analysis, there are clear points that could be drawn regarding COVID-19 transmission and social gathering.
Conclusion


The transmission of COVID-19 within the district was inevitable, however, the funeral played an important role in the early transmission and spread of infection. Funerals continue to be an ongoing source of COVID-19 super-spreader events. While funerals cannot be avoided, adherence to COVID-19 guidelines on funerals can help reduce infection transmission rates. Exploring new methods, such as virtual funeral services and virtual memorial services can help reduce the risk of COVID-19 transmission associated with funerals.
What is known about this topic
- Physical distancing is one of the best measures for COVID-19 prevention
- The elderly are most affected by COVID-19
What this study adds
- Events such as funerals and parties have the potential to become COVID-19 super spreader events
- Adults are most affected by COVID-19 in the Eastern Cape Province, South Africa
Competing interests


The authors declare no competing interests.
Authors' contributions


PS analyzed and interpreted the data, created all the figures and tables and wrote the paper, NM data collection, collation and interpretation, NT data collection, collation and interpretation, LN data collection, collation and interpretation, MN data collection, collation and interpretation, AHM data interpretation, and epidemiological analysis support, NG data interpretation, and epidemiological analysis support.
Acknowledgements


We would like to acknowledge the following stakeholders for their outstanding work in their response to the COVID-19 pandemic in the province and district: Nelson Mandela Bay District Department of Health, Eastern Cape Provincial Department of Health, and the National Institute for Communicable Disease. Dr Juno Thomas and Dr Ntsieni Ramalwa of the Centre for Enteric Diseases at the National Institute for Communicable Diseases for their epidemiological analysis support.
Figures


Figure 1: Epidemic curve of SARS-CoV-2 cases in Nelson Mandela Bay district, March - April 2020
Figure 2: Age and gender distribution of SARS-CoV-2 cases in Nelson Mandela Bay district, March - April 2020
Figure 3: Age distribution and fatality rates of SARS-CoV-2 cases in Nelson Mandela Bay, March - April 2020
Figure 4: Clusters of SARS-CoV-2 cases in Nelson Mandela Bay district, March - April 2020
References


- NICD. COVID-19 frequently asked questions 2020. NICD. 2020. Accessed Aug 2020.
- Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, Chen H, Wang D, Liu N, Liu D, Chen G, Zhang Y, Li D, Li J, Lian H, Niu S, Zhang L, Zhang J. Characteristics of COVID-19 infection in Beijing. J Infect. 2020; 80(4):401-6.https://doi.org/10.1016/j.jinf.2020.02.018 PubMed | Google Scholar
- Mullol J, Alobid I, Mariño-Sánchez F, Izquierdo-Domínguez A, Marin C, Klimek L, Wang D-Y, Liu Z. The Loss of Smell and Taste in the COVID-19 Outbreak: a Tale of Many Countries. Curr Allergy Asthma Rep. 2020; 20(10):61.https://doi.org/10.1007/s11882-020-00961-1 PubMed | Google Scholar
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, Azman AS, Reich NG, Lessler J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med. 2020; 172(9):577-82.https://doi.org/10.7326/M20-0504 . Google Scholar
- WHO. Transmission of SARS-CoV-2: implications for infection prevention precautions: scientific brief. WHO. 2020. Accessed Aug 2020. Google Scholar
- He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, Lau YC, Wong JY, Guan Y, Tan X, Mo X, Chen Y, Liao B, Chen W, Hu F, Zhang Q, Zhong M, Wu Y, Zhao L, Zhang F, Cowling BJ, Li F, Leung GM. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020; 26(5):672-5.https://doi.org/10.1038/s41591-020-0869-5 . PubMed | Google Scholar
- Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen H-L, Peiris M, Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020; 382(12):1177-9.https://doi.org/10.1056/nejmc2001737 Google Scholar
- WHO. Considerations in the investigation of cases and clusters of COVID-19: interim guidance, 2 April 2020. WHO. 2020. Accessed Jan 2022.
- Ozma MA, Maroufi P, Khodadadi E, Köse Ş, Esposito I, Ganbarov K, Dao S, Esposito S, Dal T, Zeinalzadeh E, Kafil HS. Clinical manifestation, diagnosis, prevention and control of SARS-CoV-2 (COVID-19) during the outbreak period. Infez Med. 2020; 28(2):153-65. Google Scholar
- Liu J, Liao X, Qian S, Yuan J, Wang F, Liu Y, Wang Z, Wang F-S, Liu L, Zhang Z. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020 Jun; 26(6):1320-1323.https://doi.org/10.3201/eid2606.200239 PubMed | Google Scholar
- Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic Transmission of SARS-CoV-2–Singapore, January 23-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 10; 69(14):411-415.https://doi.org/10.15585/mmwr.mm6914e1 PubMed | Google Scholar
- McGrail DJ, Dai J, McAndrews KM, Kalluri R. Enacting national social distancing policies corresponds with dramatic reduction in COVID19 infection rates. PLoS One. 2020 Jul 30; 15(7):e0236619.https://doi.org/10.1371/journal.pone.0236619 PubMed | Google Scholar
- COGTA. Disaster management act, 2002: Amendment of regulations issued in terms of Section 27 (2). South African Gorvernment. 2020. Accessed Aug 2020.
- NICD. COVID-19 Daily report.NICD. 2020. Accessed Aug 2020.
- Yao Y, Tian Y, Zhou J, Ma X, Yang M, Wang S. Epidemiological characteristics of SARS-CoV-2 infections in Shaanxi, China by 8 February 2020. Eur Respir J. 2020 Apr 23; 55(4):2000310.https://doi.org/10.1183/13993003.00310-2020 PubMed | Google Scholar
- Rosenberg ES, Dufort EM, Blog DS, Hall EW, Hoefer D, Backenson BP, Muse AT, Kirkwood JN, St. George K, Holtgrave DR, Hutton BJ, Zucker HA, New York State Coronavirus 2019 Response Team, Anand M, Kaufman A, Kuhles D, Maxted A, Newman A, Pulver W, Smith L, Sommer J, White J, Dean A, Derbyshire V, Egan C, Fuschino M, Griesemer S, Hull R, Lamson D, Laplante J, McDonough K, Mitchell K, Musser K, Nazarian E, Popowich M, Taylor J, Walsh A, Amler S, Huang A, Recchia R, Whalen E, Lewis E, Friedman C, Carrera S, Eisenstein L, DeSimone A, Morne J, Johnson M, Navarette K, Kumar J, Ostrowski S, Mazeau A, Dreslin S, Yates N, Greene D, Heslin E, Lutterloh E, Rosenthal E, Barranco M, Anand M, Kaufman A, Kuhles D, Maxted A, Newman A, Pulver W, Smith L, Sommer J, White J, Dean A, Derbyshire V, Egan C, Fuschino M, Griesemer S, Hull R, Lamson D, Laplante J, McDonough K, Mitchell K, Musser K, Nazarian E, Popowich M, Taylor J, Walsh A, Amler S, Huang A, Recchia R, Whalen E, Lewis E, Friedman C, Carrera S, Eisenstein L, DeSimone A, Morne J, Johnson M, Navarette K, Kumar J, Ostrowski S, Mazeau A, Dreslin S, Yates N, Greene D, Heslin E, Lutterloh E, Rosenthal E, Barranco M. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State–March 2020. Clin Infect Dis. 2020 Nov 5; 71(8):1953-1959.https://doi.org/10.1093/cid/ciaa549 PubMed | Google Scholar
- Riccardo F, Ajelli M, Andrianou XD, Bella A, Del Manso M, Fabiani M, Bellino S, Boros S, Urdiales AM, Marziano V, Rota MC, Filia A, D'Ancona F, Siddu A, Punzo O, Trentini F, Guzzetta G, Poletti P, Stefanelli P, Castrucci MR, Ciervo A, Di Benedetto C, Tallon M, Piccioli A, Brusaferro S, Rezza G, Merler S, Pezzotti P, the COVID-19 working group. Epidemiological characteristics of COVID-19 cases and estimates of the reproductive numbers 1 month into the epidemic, Italy, 28 January to 31 March 2020. Euro Surveill. 2020 Dec; 25(49):2000790.https://doi.org/10.2807/1560-7917.es.2020.25.49.2000790 PubMed | Google Scholar
-
Zhang X-Y, Huang H-J, Zhuang D-L, Nasser MI, Yang M-H, Zhu P, Zhao M-Y. Biological, clinical and epidemiological features of COVID-19, SARS and MERS and AutoDock simulation of ACE2. Infect Dis Poverty. 2020 Jul 20; 9(1):99.https://doi.org/10.1186/s40249-020-00691-6 PubMed | Google Scholar
- Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, Sanmartín JL, Fernández-García A, Cruz I, Fernández de Larrea N, Molina M, Rodríguez-Cabrera F, Martín M, Merino-Amador P, León Paniagua J, Muñoz-Montalvo JF, Blanco F, Yotti R, Blanco F, Gutiérrez Fernández R, Martín M, Mezcua Navarro S, Molina M, Muẽoz-Montalvo JF, Salinero Hernández M, Sanmartín JL, Cuenca-Estrella M, Yotti R, León Paniagua J, Fernández de Larrea N, Fernández-Navarro P, Pastor-Barriuso R, Pérez-Gómez B, Pollán M, Avellón A, Fedele G, Fernández-García A, Oteo Iglesias J, Pérez Olmeda MT, Cruz I, Fernandez Martinez ME, Rodríguez-Cabrera FD, Hernán MA, Padrones Fernández S, Rumbao Aguirre JM, Navarro Marí JM, Palop Borrás B, Pérez Jiménez AB, Rodríguez-Iglesias M, Calvo Gascón AM, Lou Alcaine ML, Donate Suárez I, Suárez Álvarez O, Rodríguez Pérez M, Cases Sanchís M, Villafáfila Gomila CJ, Carbo Saladrigas L, Hurtado Fernández A, Oliver A, Castro Feliciano E, González Quintana MN, Barrasa Fernández JM, Hernández Betancor MA, Hernández Febles M, Martín Martín L, López López L-M, Ugarte Miota T, De Benito Población I, Celada Pérez MS, Vallés Fernández MN, Maté Enríquez T, Villa Arranz M, Domínguez-Gil González M, Fernández-Natal I, Megías Lobón G, Muñoz Bellido JL, Ciruela P, Mas i Casals A, Doladé Botías M, Marcos Maeso MA, Pérez del Campo D, Félix de Castro A, Limón Ramírez R, Elías Retamosa MF, Rubio González M, Blanco Lobeiras MS, Fuentes Losada A, Aguilera A, Bou G, Caro Y, Marauri N, Soria Blanco LM, del Cura González I, Hernández Pascual M, Alonso Fernández R, Merino-Amador P, Cabrera Castro N, Tomás Lizcano A, Ramírez Almagro C, Segovia Hernández M, Ascunce Elizaga N, Ederra Sanz M, Ezpeleta Baquedano C, Bustinduy Bascaran A, Iglesias Tamayo S, Elorduy Otazua L, Benarroch Benarroch R, Lopera Flores J, Vázquez de la Villa A. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020 Aug 22; 396(10250):535-544.https://doi.org/10.1016/S0140-6736(20)31483-5 . Google Scholar
- Mthembu ME. Factors affecting men's health care seeking behaviour and use of services: a case study of Inanda Township, Durban 2015. University of KwaZulu-Natal; South Africa. 2015. Accessed Aug 2020.
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 May 12; 323(18):1775-1776.https://doi.org/10.1001/jama.2020.4683 Google Scholar
- Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020 Nov 19;20(1):1742.https://doi.org/10.1186/s12889-020-09826-8 PubMed | Google Scholar
- Ortiz-Prado E, Simbaña-Rivera K, Barreno LG, Diaz AM, Barreto A, Moyano C, Arcos V, Vásconez-González E, Paz C, Simbaña-Guaycha F, Molestina-Luzuriaga M, Fernández-Naranjo R, Feijoo J, Henriquez-Trujillo AR, Adana L, López-Cortés A, Fletcher I, Lowe R. Epidemiological, socio-demographic and clinical features of the early phase of the COVID-19 epidemic in Ecuador. PLoS Negl Trop Dis. 2021 Jan 4; 15(1):e0008958.https://doi.org/10.1371/journal.pntd.0008958 PubMed | Google Scholar
- Johansson MA, Quandelacy TM, Kada S, Prasad PV, Steele M, Brooks JT, Slayton RB, Biggerstaff M, Butler JC. SARS-CoV-2 transmission from people without COVID-19 symptoms. JAMA Netw Open. 2021 Jan 4; 4(1):e2035057.https://doi.org/10.1001/jamanetworkopen.2020.35057 PubMed | Google Scholar
- Zhao H, Lu X, Deng Y, Tang Y, Lu J. COVID-19: asymptomatic carrier transmission is an underestimated problem. Epidemiol Infect. 2020 Jun 11; 148:e116.https://doi.org/10.1017/s0950268820001235 PubMed | Google Scholar
- Qian G, Yang N, Ma AHY, Wang L, Li G, Chen X, Chen X. COVID-19 transmission within a family cluster by presymptomatic carriers in China. Clin Infect Dis. 2020 Jul 28;71(15):861-862. Clinical Infectious Diseases. 2020; 71(15):861-2.https://doi.org/10.1093/cid/ciaa316 . PubMed | Google Scholar
- Hamner L. High SARS-CoV-2 attack rate following exposure at a choir practice–Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020 May 15; 69(19):606-610.http://dx.doi.org/10.15585/mmwr.mm6919e6 . Google Scholar
-
Ghinai I, Woods S, Ritger KA, McPherson TD, Black SR, Sparrow L, Fricchione MJ, Kerins JL, Pacilli M, Ruestow PS, Arwady MA, Beavers SF, Payne DC, Kirking HL, Layden JE. Community Transmission of SARS-CoV-2 at Two Family Gatherings - Chicago, Illinois, February-March 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 17;69(15):446-450.https://doi.org/10.15585/mmwr.mm6915e1 PubMed | Google Scholar
- Madisa K. Funerals big source of Eastern Cape Covid-19 infections. Sowetanlive. 2020. Accessed Aug 2020.
- Shange N. Covid-19: Bloemfontein church that hosted infected guests says they were screened on arrival in SA. Timeslive. 2020. Accessed Aug 2020.
- Kimberly M. Two funerals - 54 people infected with Covid-19, one dead. Sowetanlive. 2020. Accessed Aug 2020.
- Yong SEF, Anderson DE, Wei WE, Pang J, Chia WN, Tan CW, Teoh YL, Rajendram P, Toh MPHS, Poh C, Koh VTJ, Lum J, Suhaimi N-AM, Chia PY, Chen MI-C, Vasoo S, Ong B, Leo YS, Wang L, Lee VJM. Connecting clusters of COVID-19: an epidemiological and serological investigation. Lancet Infect Dis. 2020 Jul; 20(7):809-815.https://doi.org/10.1016/S1473-3099(20)30273-5 . Google Scholar
- Pung R, Chiew CJ, Young BE, Chin S, Chen MI-C, Clapham HE, Cook AR, Maurer-Stroh S, Toh MPHS, Poh C, Low M, Lum J, Koh VTJ, Mak TM, Cui L, Lin RVTP, Heng D, Leo Y-S, Lye DC, Lee VJM, Kam K, Kalimuddin S, Tan SY, Loh J, Thoon KC, Vasoo S, Khong WX, Suhaimi N-A, Chan SJ, Zhang E, Oh O, Ty A, Tow C, Chua YX, Chaw WL, Ng Y, Abdul-Rahman F, Sahib S, Zhao Z, Tang C, Low C, Goh EH, Lim G, Hou Y, Roshan I, Tan J, Foo K, Nandar K, Kurupatham L, Chan PP, Raj P, Lin Y, Said Z, Lee A, See C, Markose J, Tan J, Chan G, See W, Peh X, Cai V, Chen WK, Li Z, Soo R, Chow AL, Wei W, Farwin A, Ang LW. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020 Mar 28; 395(10229):1039-1046.https://doi.org/10.1016/S0140-6736(20)30528-6 . Google Scholar
- Ryan M. In defence of digital contact-tracing: human rights, South Korea and Covid-19. International Journal of Pervasive Computing and Communications. 2020 Aug 6.https://doi.org/10.1108/IJPCC-07-2020-0081 Google Scholar
- Carr D, Boerner K, Moorman S. Bereavement in the time of coronavirus: Unprecedented challenges demand novel interventions. J Aging Soc Policy. 2020 Jul-Oct; 32(4-5):425-431.https://doi.org/10.1080/08959420.2020.1764320 . Google Scholar
- Muturi I, Freeman S, Banner D. Reply to: Comment on: Virtual funerals: A feasible and safer option during the COVID-19 pandemic. J Am Geriatr Soc. 2021 Apr; 69(4):882-883.https://doi.org/10.1111/jgs.17042 PubMed | Google Scholar
- Mboya IB, Ngocho JS, Mgongo M, Samu LP, Pyuza JJ, Amour C, Mahande MJ, Leyaro BJ, George JM, Philemon RN, Muro F, Renju J, Msuya SE. Community engagement in COVID-19 prevention: experiences from Kilimanjaro region, Northern Tanzania. Pan Afr Med J. 2020 Aug 14; 35(Suppl 2):146.https://doi.org/10.11604/pamj.supp.2020.35.146.24473 PubMed | Google Scholar
- Weinberger-Litman SL, Litman L, Rosen Z, Rosmarin DH, Rosenzweig C. A look at the first quarantined community in the USA: Response of religious communal organizations and implications for public health during the COVID-19 pandemic. J Relig Health. 2020 Oct; 59(5):2269-2282.https://doi.org/10.1007/s10943-020-01064-x . PubMed | Google Scholar
- Zhu J, Cai Y. Engaging the communities in Wuhan, China during the COVID-19 outbreak. Global health research and policy. 2020; 5(1):1-4.https://doi.org/10.1186/s41256-020-00162-3 . PubMed | Google Scholar